|
 |
- Search
| Korean J Helicobacter Up Gastrointest Res > Volume 23(1); 2023 > Article |
|
Question: A 54-year-old woman was referred to our tertiary center for further evaluation of an esophageal subepithelial tumor (SET) that had been incidentally found during screening endoscopy. The tumor was located in the mid-esophagus and was covered by normal esophageal mucosa (Fig. 1A). According to the patientŌĆÖs history, the esophageal SET was initially detected at another local medical center 2 years ago. The center may have planned a patient follow-up according to the current practice guidelines, which state that small esophageal SET can be managed by periodic surveillance endoscopy [1]. However, the patient visited another local medical center that considered the SET as a newly discovered lesion and referred her to our center. The size of the esophageal SET increased slightly on endoscopic image. EUS revealed a homogenous hypoechoic lesion measuring 1.0├Ś0.5 cm in the third layer of the esophagus (Fig. 1B).
What is the most likely diagnosis?
Answer: We performed an underwater endoscopic mucosal resection (UW-EMR). A 15-mm polypectomy snare (Endo-Flex GmbH, Voerde, Germany) was introduced through a two-channel endoscope (GIF-2TQ260M; Olympus, Tokyo, Japan) that enables the insertion of a snare through an endoscopic channel while maintaining water infusion to completely immerse the tumor. The table was tilted by approximately 15┬░ to prevent aspiration during the procedure. En-bloc resection was achieved. The operative time was 4 minutes. There was no sign of esophageal perforation or residual lesion. The resection margin was negative for tumor cells and lymphovascular invasion. The histological diagnosis revealed esophageal adenoid cystic carcinoma (EACC) of the cribriform type (Fig. 2). Abdominal and chest CT revealed no evidence of lymph node metastasis.
The patient wanted an early follow-up, although the risk of lymph node metastasis in early EACC is not well known. Hence, periodic surveillance using endoscopy and chest CT was planned. Endoscopic biopsy from the resected site 3 months after the procedure revealed no residual tumor. Although the patient might have a good prognosis during follow-up, meticulous follow-up plan is still needed.
Adenoid cystic carcinoma is a malignant tumor that most frequently occurs in salivary glands. EACC is rare and accounts for only 0.1% of all esophageal malignancies [2,3]. Dysphagia is the most common symptom. Often, metastases are detected during diagnosis [2]. Endoscopic findings of early stage EACC include small SETs covered with normal mucosa that makes early diagnosis difficult. Previous reports on early stage EACC demonstrated no esophageal symptoms [2,3]. Hence, EUS can be helpful in distinguishing early stage EACC from benign tumors such as leiomyoma.
The treatment of choice for EACC is radical resection with regional lymph node dissection [4]. Histologically, adenoid cystic carcinoma shows three different cellular patterns: cribriform, tubular, and solid [5]. The solid pattern is associated with poorer prognosis than the other two patterns. Moreover, lymph node metastasis and vascular invasion, are associated with poor prognosis [5].
The association of lymph node metastasis with EACC invasion depth is not well known. A recent study reported that lymph node metastasis was found in only 4% of patients (1/25) with EACC who had submucosal or mucosal invasion [4]. In two cases, submucosal invasive EACC was treated by endoscopic resections including endoscopic enucleation and endoscopic submucosal dissection with a good prognosis without additional treatment [2,3,5].
Recently, UW-EMR for esophageal SET in the third layer was introduced as an effective and safe treatment modality with reduced procedure time and complication risk [6]. Therefore, we performed UW-EMR and achieved a complete en-bloc resection.
Acknowledgements
This study was supported by the 2022 overseas training grant from Pusan National University Yangsan Hospital.
Fig.┬Ā1.
(A) Endoscopic image showing an incidentally detected midesophageal subepithelial tumor covered with normal mucosa. (B) Endoscopic ultrasonographic image showing a homogenous hypoechoic lesion measuring 1.0├Ś0.5 cm in the third layer of the esophagus.
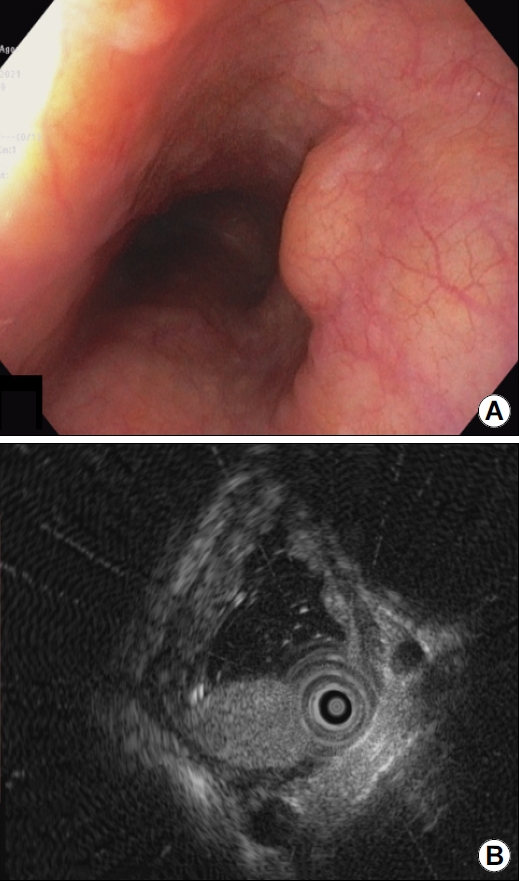
Fig.┬Ā2.
(A) Microscopic image of the resected tissue showing the cribriform structure of the tumor cells (H&E stain, ├Ś40). (B) Image showing appearance of the tumor cells using the p63 stain (├Ś200). (C) Image showing appearance of the tumor cells using the S100 stain (├Ś200). (D) Image showing appearance of tumor cells using the cytokeratin 7 (CK7) stain (├Ś200).

REFERENCES
1. Cho JW. Current guidelines in the management of upper gastrointestinal subepithelial tumors. Clin Endosc 2016;49:235ŌĆō240.




2. Yoshikawa K, Kinoshita A, Hirose Y, et al. Endoscopic submucosal dissection in a patient with esophageal adenoid cystic carcinoma. World J Gastroenterol 2017;23:8097ŌĆō8103.



3. Na YJ, Shim KN, Kang MJ, et al. Primary esophageal adenoid cystic carcinoma. Gut Liver 2007;1:178ŌĆō181.



4. Sawada G, Moon J, Saito A, et al. A case of adenoid cystic carcinoma of the esophagus. Surg Case Rep 2015;1:119.




-
METRICS

-
- 0 Crossref
- 1,173 View
- 46 Download
- Related articles in Korean J Helicobacter Up Gastrointest Res
-
Approach to Small Gastric Subepithelial Lesions2023 March;23(1)
Common Gastric Subepithelial Tumors in Koreans2022 March;22(1)
A Missing Subepithelial Tumor in the Duodenum2020 December;20(4)