|
 |
- Search
| Korean J Helicobacter Up Gastrointest Res > Volume 22(3); 2022 > Article |
|
Abstract
Achalasia is characterized by peristaltic failure and incomplete relaxation of the lower esophageal sphincter. The incidence and prevalence of achalasia increase with age, although achalasia can affect all age groups. The pathophysiology of achalasia involves the loss of inhibitory ganglion cells in the myenteric plexus of the esophagus. Its main symptoms include dysphagia, chest pain, regurgitation, and weight loss. The method of diagnosing achalasia has evolved from conventional manometry in the 1970s to high-resolution manometry in the 2010s. High-resolution manometry based on spatiotemporal plots can diagnose achalasia more precisely than conventional manometry. Moreover, novel parameters such as integrated relaxation pressure (IRP) (according to the Chicago classification) have increased diagnostic accuracy. However, cases of achalasia presenting with normal IRP have been reported. Therefore, the novel Chicago classification version 4.0 has adopted additional tests. These tests include the stress test for esophageal motor disorders, timed barium esophagography, and test using a functional lumen imaging probe that measures the distensibility of the esophagogastric junction. Achalasia was previously treated using surgical myotomy, balloon dilation, and botulinum toxin injection. However, peroral endoscopic myotomy (POEM) has recently become the mainstay treatment. POEM has a higher clinical success rate and a lower complication rate than surgical myotomy. Esophageal cancer and pulmonary conditions such as aspiration pneumonia are possible complications of achalasia. In this review, the current knowledge regarding achalasia together with novel diagnostic and therapeutic strategies are discussed.
ņŗØļÅäļŖö ņŗØĻ┤┤ļź╝ ņāüļČĆņŗØļÅäņĪ░ņ×äĻĘ╝ņŚÉņä£ ĒĢśļČĆņŗØļÅäņĪ░ņ×äĻĘ╝Ļ╣īņ¦Ć ņŚ░ļÅÖņÜ┤ļÅÖņØä ĒåĄĒĢ┤ ļé┤ļĀż ļ│┤ļé┤ļŖö ņØĖņ▓┤ ĻĖ░Ļ┤ĆņØ┤ļŗż. ņŗØļÅä ņØ┤ņÖäļČłļŖź(achalasia)ņØĆ ĒĢśļČĆņŗØļÅäņĪ░ņ×äĻĘ╝ņØś ļ╣äņĀĢņāüņĀüņØĖ ņłśņČĢņ£╝ļĪ£ ņĀĢņāüņĀüņØĖ ņŚ░ļÅÖņÜ┤ļÅÖņØ┤ ņØ┤ļŻ©ņ¢┤ņ¦Ćņ¦Ć ņĢŖņĢä ņé╝Ēé┤Ļ│żļ×ĆņØ┤ļéś ļ╣äņŗ¼ņØĖņä▒ ĒØēĒåĄ ļō▒ņØä ņ£Āļ░£ĒĢ£ļŗż[1]. ņŗØļÅä ņØ┤ņÖäļČłļŖźņØĆ ņśłņĀäļČĆĒä░ ņĢīļĀżņĀĖ ņ׳ļŹś ņ¦łļ│æņØ┤ļéś, Ļ│ĀĒĢ┤ņāüļÅä ļé┤ņĢĢ Ļ▓Ćņé¼ ļ░Å ņŚ¼ļ¤¼ Ļ░Ćņ¦Ć ņ¦äļŗ© ļ░®ļ▓ĢņØś ļ╣äņĢĮņĀüņØĖ ļ░£ņĀäņ£╝ļĪ£ ņØĖĒĢśņŚ¼ ņĄ£ĻĘ╝ ļŹöņÜ▒ Ļ░üĻ┤æļ░øĻ│Ā ņ׳ņ£╝ļ®░, 2010ļģäļīĆ ņØ┤Ēøä Ļ▓ĮĻĄ¼ņĀü ļé┤ņŗ£Ļ▓Į ĻĘ╝ņĀłĻ░£ņłĀ ļō▒ņØś ņāłļĪ£ņÜ┤ ņ╣śļŻī ļ░®ļ▓ĢņØ┤ Ļ░£ļ░£ļÉśņ¢┤ ņ¦łļ│æņØś ņĀĢĒÖĢĒĢ£ ņ¦äļŗ© ļ░Å ņ╣śļŻīņŚÉ ļīĆĒĢ┤ņä£ ĻĘĖ ņ¢┤ļŖÉ ļĢīļ│┤ļŗż Ļ┤Ćņŗ¼ņØ┤ ņ¦æņżæļÉśĻ│Ā ņ׳ļŗż. ļ│Ė ņøÉĻ│ĀņŚÉņä£ļŖö ņŗØļÅä ņØ┤ņÖäļČłļŖźņØś ņ¦äļŗ©ņŚÉ ņō░ņØ┤ļŖö ņŗØļÅä ļé┤ņĢĢ Ļ▓Ćņé¼ņŚÉņä£ ņĄ£ĻĘ╝ ņāłļĪŁĻ▓ī ņĀ£ņŗ£ļÉ£ ņŗ£ņ╣┤Ļ│Ā ĻĖ░ņżĆ 4.0Ļ│╝ ņ╣śļŻīņŚÉ ļīĆĒĢ£ ņāłļĪ£ņÜ┤ ņŚ░ĻĄ¼ Ļ▓░Ļ│╝ļōżņØä ņåīĻ░£ĒĢśĻ│Āņ×É ĒĢ£ļŗż[2].
ņŗØļÅä ņØ┤ņÖäļČłļŖźņØĆ 1672ļģä ņśüĻĄŁņØś ņØśņé¼ WillisņŚÉ ņØśĒĢ┤ ņ▓śņØī ņĢīļĀżņ¦ä ņ¦łļ│æņ£╝ļĪ£, ļŗ╣ņŗ£ņŚÉļŖö ņøÉņØĖņØä ņל ņĢī ņłś ņŚåļŖö ņŗØļÅäņłśņČĢņØ┤ ņ׳ļŖö ĒÖśņ×ÉņŚÉņä£ Ļ│Āļלļ╝łņŚÉ ņŖżĒÄĆņ¦Ćļź╝ ļČÖņŚ¼ņä£ ņŗØļÅäļź╝ ļäōĒśĆņä£ ņ╣śļŻīļź╝ Ē¢łļŗżĻ│Ā ĒĢ£ļŗż[3]. ļö░ļØ╝ņä£ ņŗØļÅäļé┤ņĢĢ Ļ▓Ćņé¼Ļ░Ć ļÅäņ×ģļÉśĻĖ░ ņĀäļČĆĒä░ ņØ┤ļ»Ė ņŗØļÅä ņØ┤ņÖäļČłļŖźņŚÉ ļīĆĒĢ┤ ņØĖņ¦ĆĒĢśĻ│Ā ņ׳ņŚłļŗżĻ│Ā ņāØĻ░üļÉśļ®░ ņØ┤ļ»Ė ņłśļ░▒ ļģä ņĀäļČĆĒä░ ņĪ┤ņ×¼Ē¢łļŹś ņ¦łļ│æņØ┤ļØ╝Ļ│Ā ĒĢĀ ņłś ņ׳ļŗż[3]. ņØ┤ņĀ£ļŖö ņŗØļÅäņÜ┤ļÅÖ ņ¦łĒÖśņØś ņ¦äļŗ©ņŚÉ Ļ░Ćņן ņżæņÜöĒĢ£ Ļ▓Ćņé¼ļĪ£ ņŚ¼Ļ▓©ņ¦ĆļŖö ņŗØļÅäļé┤ņĢĢ Ļ▓Ćņé¼ļŖö 1970ļģäļīĆņŚÉ ņ▓śņØī ņ×äņāüņŚÉ ņåīĻ░£ļÉśņŚłļŗż. ņāłļĪ£ņÜ┤ ĒīÉļÅģ ĻĖ░ņżĆņØ┤ ļéśņś¼ ļĢīļ¦łļŗż ņłśņŗ£ļĪ£ ņ¦äļŗ©ļ¬ģņØ┤ ļ░öļĆīĻ▒░ļéś ĒśĖļæÉĻ╣īĻĖ░ ņŗØļÅäņ▓śļ¤╝ ņ¦äļŗ©ļ¬ģņØ┤ ņé¼ļØ╝ņ¦ĆļŖö ļō▒ņØś ņŗ£Ē¢ēņ░®ņśżļź╝ Ļ▓¬ĻĖ░ļÅä ĒĢśņśĆĻ│Ā, ņŗØļÅäļé┤ņĢĢ Ļ▓Ćņé¼ļź╝ ĒåĄĒĢ£ ņŗØļÅäņÜ┤ļÅÖņ¦łĒÖśņØś ņ¦äļŗ©ļ¬ģņØ┤ ņ×äņāü ņ”ØņāüĻ│╝ Ļ┤┤ļ”¼Ļ░Ć ņ׳ņŚłĻĖ░ņŚÉ ņŗ£ņ╣┤Ļ│Ā 4.0ļČĆĒä░ļŖö ņ×äņāüņĀüņØĖ ņ”ØņāüņØ┤ ņ׳ņØä ļĢīļ¦ī ĒĢ┤ļŗ╣ ņ¦äļŗ©ļ¬ģņØä ļČÖņØ┤ļÅäļĪØ ĒĢśļŖö ļō▒ņØś ļ│ĆĒÖöļź╝ Ļ▓¬ņŚłļŗż. ĻĘĖļ¤¼ļéś ņŗØļÅä ņØ┤ņÖäļČłļŖźņØĆ ņØ┤ļ¤¼ĒĢ£ ļ│ĆĒÖöņŚÉļÅä ļČłĻĄ¼ĒĢśĻ│Ā ļÜ£ļĀĘĒĢ£ ņ¦äļŗ©ļ¬ģņ£╝ļĪ£ ņ×Éļ”¼ļ¦żĻ╣ĆĒĢśņśĆļŗż[4].
ņŗØļÅä ņØ┤ņÖäļČłļŖźņØĆ ļīĆļץņĀüņ£╝ļĪ£ ņĀäņäĖĻ│ä ņØĖĻĄ¼ 10ļ¦ī ļ¬ģļŗ╣ 1~5ļ¬ģ ņĀĢļÅäņØś ļ░£ņāØļźĀ(incidence)ņØä ļ│┤ņØĖļŗżĻ│Ā ņĢīļĀżņĀĖ ņ׳Ļ│Ā, ņ£Āļ│æļźĀ(prevalence)ņØĆ ņØĖĻĄ¼ 10ļ¦ī ļ¬ģļŗ╣ 7~32ļ¬ģ ņĀĢļÅäļØ╝Ļ│Ā ņĢīļĀżņĀĖ ņ׳ļŗż[5-7]. ĒĢśņ¦Ćļ¦ī Ļ│ĀņŗØņĀü ļé┤ņĢĢ Ļ▓Ćņé¼Ļ░Ć ņō░ņśĆļŹś 1970~1990ļģäļīĆļ│┤ļŗż Ļ│ĀĒĢ┤ņāüļÅä ļé┤ņĢĢ Ļ▓Ćņé¼Ļ░Ć ĒÖ£ņä▒ĒÖöļÉ£ 2010ļģä ņØ┤Ēøä ņ¦äļŗ©ņ£©ņØ┤ ļåÆņĢäņĪīļŗżļŖö ļ│┤Ļ│ĀļÅä ņä£ĻĄ¼ ņ¬ĮņØä ņżæņŗ¼ņ£╝ļĪ£ ļéśņśżĻ│Ā ņ׳ļŗż[8,9]. ĒĢ£ĻĄŁņŚÉņä£ļŖö Ļ▒┤Ļ░Ģļ│┤ĒŚśņŗ¼ņé¼ĒÅēĻ░ĆņøÉ ņ×ÉļŻīļź╝ ļ░öĒāĢņ£╝ļĪ£ ĒĢ£ 2011ļģäņŚÉ ļ░£Ēæ£ļÉ£ ņŚ░ĻĄ¼ņŚÉ ļö░ļź┤ļ®┤, ņØĖĻĄ¼ 10ļ¦ī ļ¬ģļŗ╣ ļé©ņ×ÉļŖö 0.33, ņŚ¼ņ×ÉļŖö 0.44ņØś ļ░£ņāØļźĀņØä ļ│┤Ļ│ĀĒĢśĻ│Ā ņ׳ļŗż[10]. ņŗØļÅä ņØ┤ņÖäļČłļŖźņØĆ ņĀä ņŚ░ļĀ╣ļīĆņŚÉņä£ ļ░£ņāØĒĢĀ ņłś ņ׳ņ£╝ļéś, ļ░£ņāØļźĀĻ│╝ ņ£Āļ│æļźĀ ļ¬©ļæÉ 50ņäĖ ņØ┤ņāüņØś Ļ│ĀļĀ╣ņĖĄņŚÉņä£ ņ”ØĻ░ĆĒĢ£ļŗżĻ│Ā ņĢīļĀżņĀĖ ņ׳ļŗż[7,9,11].
ņĢäņ¦üĻ╣īņ¦ĆļÅä ĻĘĖ ņĀĢĒÖĢĒĢ£ ņøÉņØĖņØĆ ļ░ØĒśĆņĀĖ ņ׳ņ¦Ć ņĢŖņ£╝ļéś, ņØ╝ļČĆ ņŚ░ĻĄ¼ņŚÉņä£ ĒŖ╣ņĀĢ HLA ņ£ĀņĀäņ×ÉĒśĢņØ┤ ņ׳ļŖö ĒÖśņ×ÉļōżņŚÉĻ▓ī ļ░öņØ┤ļ¤¼ņŖż Ļ░ÉņŚ╝ ņØ┤Ēøä ņŗØļÅä ņØ┤ņÖäļČłļŖźņ£╝ļĪ£ ļ░£ĒśäĒĢ£ļŗżļŖö Ļ░ĆņäżņØä ņĀ£ņŗ£ĒĢ£ ļ░ö ņ׳Ļ│Ā ĒŖ╣ņĀĢ ņ£ĀņĀäņ¦łĒÖś(triple A syndrome)Ļ│╝ņØś Ļ┤ĆļĀ©ņä▒ņŚÉ ļīĆĒĢ£ ņŚ░ĻĄ¼ļÅä ņ׳ņŚłņ£╝ļéś ņØ╝ļ░śĒÖöĒĢśņ¦ĆļŖö ļ¬╗ĒĢśņśĆļŗż[1,5,12,13]. ņĄ£ĻĘ╝ņŚÉļŖö ĒśĖņé░ĻĄ¼ņä▒ ņŗØļÅäņŚ╝Ļ│╝ņØś Ļ┤ĆļĀ©ņä▒ņŚÉ ļīĆĒĢ┤ņä£ļÅä ņŚ¼ļ¤¼ ņŚ░ĻĄ¼Ļ░Ć ņØ┤ļŻ©ņ¢┤ņ¦ĆĻ│Ā ņ׳ņ£╝ļéś, ņĢäņ¦üĻ╣īņ¦Ć ĻĘĖ Ļ┤ĆļĀ©ņä▒ņØĆ ļ¬ģĒÖĢĒĢśņ¦Ć ņĢŖļŗż[14,15]. ļĖīļØ╝ņ¦ł Ļ░ÖņØĆ ĒŖ╣ņĀĢ ņ¦ĆņŚŁņŚÉņä£ļŖö ņāżĻ░ĆņŖż(Chagas) ļ│æņØś ņ”Øņāü ņżæņØś ĒĢśļéśļĪ£ ļéśĒāĆļéśĻĖ░ļÅä ĒĢ£ļŗż[5]. ņŗØļÅä ņØ┤ņÖäļČłļŖź ĒÖśņ×ÉļōżņŚÉņä£ ņāüļīĆņĀüņ£╝ļĪ£ ņ×ÉĻ░Ćļ®┤ņŚŁņ¦łĒÖś ņ£Āļ│æļźĀņØ┤ ļåÆļŗżĻ│Ā ņĢīļĀżņĀĖ ņ׳ņ¢┤, ņČöĻ░ĆņĀüņØĖ ņŚ░ĻĄ¼Ļ░Ć ĻĖ░ļīĆļÉśĻ│Ā ņ׳ļŗż[16,17]. ļ│æĒā£ ņÜöņØĖņ£╝ļĪ£ļŖö ĒĢśļČĆņŗØļÅäņĪ░ņ×äĻĘ╝Ļ│╝ ĒĢśļČĆņŗØļÅä ĻĘ╝ņ£ĪņĖĄņØś ĻĘ╝ņ£ĪņĖĄņ¢╝ĻĖ░(myenteric plexus ganglion)ņØś ĻĖ░ļŖź ņåīņŗżņØ┤ ņøÉņØĖņØ╝ Ļ▓āņ£╝ļĪ£ ņČöņĀĢĒĢśĻ│Ā ņ׳ļŗż[5].
Ļ░Ćņן ĒØöĒĢ£ ņ”ØņāüņØĆ ņé╝Ēé┤Ļ│żļ×ĆņØ┤ļ®░, Ļ│ĀĒśĢņŗØĻ│╝ ņ£ĀļÅÖņŗØņŚÉ ļÅÖņŗ£ņŚÉ ņ׳ļŗżļŖö Ļ▓āņØ┤ ĒŖ╣ņ¦ĢņĀüņØ┤ļŗż. ņåīĒÖö ņĢł ļÉ£ ņØīņŗØņØ┤ ņŚŁļźśĒĢ┤ņä£ ņś¼ļØ╝ņśżļŖö Ļ▓āļÅä ņŻ╝ņÜö ņ”Øņāü ņżæņØś ĒĢśļéśņØ┤ļ®░ ĒŖ╣Ē׳ ņĢ╝Ļ░äņŚÉ ļłäņøī ņ׳ņØä ļĢī ņŚŁļźśĻ░Ć ņŗ¼ĒĢśļŗżĻ│Ā ĒĢ£ļŗż[5]. ņŚŁļźś ņ”Øņāüņ£╝ļĪ£ ņØĖĒĢśņŚ¼ ņ£äņŗØļÅä ņŚŁļźśļĪ£ ņśżņØĖĒĢśļŖö Ļ▓ĮņÜ░ļÅä ņ׳ņ£╝ļ»ĆļĪ£ ņŻ╝ņØśļź╝ ņÜöĒĢ£ļŗż[18,19]. ņŚŁļźś ļ░Å ņé╝Ēé┤Ļ│żļ×Ć ļō▒ņ£╝ļĪ£ ņØĖĒĢśņŚ¼ ņ▓┤ņżæ Ļ░ÉņåīĻ░Ć ļÅÖļ░śļÉśĻĖ░ļÅä ĒĢśĻ│Ā, Ļ░äĒś╣ ĒØĪņØĖņä▒ ĒÅÉļĀ┤ņØ┤ ļ░śļ│ĄļÉśĻĖ░ļÅä ĒĢ£ļŗż[19]. ĒØēĒåĄļÅä ĒŖ╣ņ¦ĢņĀüņØĖ ņ”ØņāüņØĖļŹ░ ĒŖ╣Ē׳ 3ĒśĢ ņŗØļÅä ņØ┤ņÖäļČłļŖźņŚÉņä£ ļŹö ļÅäļō£ļØ╝ņ¦äļŗżĻ│Ā ņĢīļĀżņĀĖ ņ׳ļŗż[5]. ĒØēĒåĄņØś ĻĖ░ņĀäņØĆ ņĢäņ¦üļÅä ļ¬ģĒÖĢĒĢśņ¦Ć ņĢŖņ£╝ļéś, ņŗØļÅä ļé┤Ļ░Ģ ļé┤ņŚÉ ļ©Ėļ¼╝ļ¤¼ ņ׳ļŖö ņØīņŗØļ¼╝ņØś ļ░£ĒÜ©ņŚÉ ņØśĒĢ£ ņŗØļÅä ļé┤Ļ░ĢņØś ĒÖöĒĢÖņłśņÜ®ņ▓┤ ņ×ÉĻĘ╣ņŚÉ ņØśĒĢ£ Ļ▓āņØ┤ļØ╝ļŖö Ļ░Ćņäż, ņŗØļÅä ļ»╝ļ¼┤ļŖ¼ ĻĘ╝ņ£ĪņØś ļČłĒśæ ņłśņČĢņŚÉ ņØśĒĢ£ Ļ▓āņØ┤ļØ╝ļŖö Ļ░Ćņäż ļō▒ņØ┤ ņĀ£ņŗ£ļÉśĻ│Ā ņ׳ļŗż[5]. ļīĆĒæ£ņĀüņØĖ ņ”ØņāüņØĖ ņé╝Ēé┤Ļ│żļ×Ć, ņØīņŗØļ¼╝ ņŚŁļźś, ĒØēĒåĄ, ņ▓┤ņżæ Ļ░Éņåīļź╝ ļ¼Čņ¢┤ņä£ Eckardt ņĀÉņłśĻ░Ć ņ╣śļŻī ņĀäĒøä ĒÜ©Ļ│╝ ĒīÉņĀĢņŚÉ ļäÉļ”¼ ņō░ņØ┤Ļ│Ā ņ׳ņ£╝ļéś, ņŗżņĀ£ ņ”ØņāüņØä ņל ļ░śņśüĒĢśņ¦Ć ļ¬╗ĒĢ£ļŗżļŖö ļ░śļĪĀļÅä ņĀ£ņŗ£ļÉśĻ│Ā ņ׳ļŗż[5,20]. Eckardt ņĀÉņłśļŖö ņé╝Ēé┤Ļ│żļ×Ć, ņŚŁļźś, ĒØēĒåĄņØä Ļ░üĻ░ü ņŚåņ£╝ļ®┤ 0ņĀÉ, Ļ░äĒś╣ ņ׳ņ£╝ļ®┤ 1ņĀÉ, ļ¦żņØ╝ ņ׳ņ£╝ļ®┤ 2ņĀÉ, ņŗØņé¼ ļĢīļ¦łļŗż ņ׳ņ£╝ļ®┤ 3ņĀÉņ£╝ļĪ£ ĒĢśĻ│Ā, ņ▓┤ņżæ Ļ░ÉņåīĻ░Ć ņŚåņ£╝ļ®┤ 0ņĀÉ, 5 kg ļ»Ėļ¦īņØ┤ļ®┤ 1ņĀÉ, 5~10 kgņØ┤ļ®┤ 2ņĀÉ, 10 kg ņ┤łĻ│╝ņØ┤ļ®┤ 3ņĀÉņ£╝ļĪ£ ĒĢśņŚ¼ ņ┤Ø 12ņĀÉ ļ¦īņĀÉņ£╝ļĪ£ ĒÅēĻ░ĆĒĢ£ļŗż.
ņāüļČĆ ļé┤ņŗ£Ļ▓ĮņØĆ ņ¦äļŗ©ņ£©ņØ┤ ļé«ļŗżĻ│Ā ņĢīļĀżņĀĖ ņ׳Ļ│Ā, ĒŖ╣Ē׳ ņŗØļÅä ņØ┤ņÖäļČłļŖź ņ┤łĻĖ░ņŚÉļŖö ņ¦äļŗ©ņŚÉ Ēü░ ļÅäņøĆņØ┤ ņĢł ļÉśļŖö Ļ▓āņ£╝ļĪ£ ņĢīļĀżņĀĖ ņ׳ļŗż[19,21]. ļé┤ņŗ£Ļ▓Į Ļ▓Ćņé¼ņŚÉ ņØĄņłÖĒĢ£ ņĀäļ¼ĖĻ░ĆņØ╝ņ¦ĆļØ╝ļÅä ņ£äņŗØļÅä Ļ▓ĮĻ│äļČĆ ņ¦üņāüļ░®ņŚÉņä£ ļé┤ņŗ£Ļ▓Į Ļ┤Ćņ░░ ņżæņŚÉ ņåĪĻĖ░ļź╝ ĒĢśļŗż ļ│┤ļ®┤ ņ£äņŗØļÅä Ļ▓ĮĻ│äļČĆĻ░Ć ņåÉņēĮĻ▓ī ņŚ┤ļ”¼ĻĖ░ ļĢīļ¼ĖņŚÉ ņØ╝ļ░śņĀüņØĖ ļé┤ņŗ£Ļ▓Į Ļ▓Ćņé¼ņŚÉņä£ļŖö ņŗØļÅä ņØ┤ņÖäļČłļŖźņØä ļåōņ╣śļŖö Ļ▓ĮņÜ░ļÅä ņóģņóģ ņ׳ļŗż. ĒĢśņ¦Ćļ¦ī ņŗØļÅä Ēśæņ░®ņØä ņØ╝ņ£╝ĒéżļŖö 2ņ░©ņĀüņØĖ ņøÉņØĖ Ļ░Éļ│äņŚÉ ļÅäņøĆņØ┤ ļÉĀ Ļ▓āņ£╝ļĪ£ ņāØĻ░üļÉśĻ│Ā ņ׳ļŗż[21]. ļśÉĒĢ£, ļé┤ņŗ£Ļ▓Į Ļ┤Ćņ░░ ņŗ£ņŚÉ ņŗØļÅä ļé┤Ļ░ĢņŚÉ ļ╣äņĀĢņāüņĀüņ£╝ļĪ£ ņØīņŗØļ¼╝ņØ┤ļéś ņĢĪņ▓┤ļźśĻ░Ć Ļ│ĀņŚ¼ ņ׳ļŗżĻ▒░ļéś ņŗØļÅä ļé┤Ļ░ĢņØ┤ ļŖśņ¢┤ļéś ņ׳ļŗżļ®┤ ņŗØļÅä ņØ┤ņÖäļČłļŖźņØä ņØśņŗ¼ĒĢĀ ņłś ņ׳ļŗż[21].
1970ļģäļīĆņŚÉ ļÅäņ×ģļÉ£ Ļ│ĀņŗØņĀü ļé┤ņĢĢ Ļ▓Ćņé¼ļŖö ļŗ╣ņŗ£ļ¦ī ĒĢ┤ļÅä ļ¼╝ņØ┤ ĒØśļ¤¼ļéśņśżļŖö Ļ┤Ćļźś ņĖĪņĀĢĻ┤Ćņ£╝ļĪ£ ņØ┤ļŻ©ņ¢┤ņ¦ä Ļ▓Ćņé¼Ļ░Ć ņŻ╝ļĪ£ ņō░ņśĆņ£╝ļ®░ ņŗØļÅä ņĢĢļĀźņØä ņĖĪņĀĢĒĢśļŖö ņä╝ņä£Ļ░Ć ņ╣┤ĒģīĒä░ļ¦łļŗż ņ░©ņØ┤ļŖö ņ׳ņ£╝ļéś ļīĆņ▓┤ņĀüņ£╝ļĪ£ 3~5 cm Ļ░äĻ▓®ņ£╝ļĪ£ ļØäņŚäļØäņŚä ļ░░ņŚ┤ļÉśņ¢┤ ņ׳ņ¢┤ņä£ ņŗØļÅä ņØ┤ņÖäļČłļŖźņ”ØņØś ĒĢĄņŗ¼ņĀüņØĖ ņ¦äļŗ©ņØĖ ĒĢśļČĆņŗØļÅäņĪ░ņ×äĻĘ╝ņØś ņØ┤ņÖä ņŚ¼ļČĆļź╝ ĒīÉļÅģĒĢśļŖö ļŹ░ ņ¢┤ļĀżņøĆņØ┤ ļ¦ÄņĢśļŗż[22]. ņ”ē, ĒĢśļČĆņŗØļÅäņĪ░ņ×äĻĘ╝ ņŻ╝ļ│ĆņØś ņä╝ņä£ņŚÉņä£ ņŗØļÅä ļ░Å ņŻ╝ļ│Ć ĻĄ¼ņĪ░ļ¼╝ņØĖ ĒÜĪĻ▓®ļ¦ēņØ┤ ņśżļź┤ļØĮļé┤ļ”¼ļØĮĒĢśļ®┤ ĒĢśļČĆņŗØļÅäņĪ░ņ×äĻĘ╝ņØ┤ Ļ▒░ņ¦ō ņØ┤ņÖäļÉśļŖö Ļ▓āņ£╝ļĪ£ ĒīÉļÅģĒĢśļŖö Ļ▓ĮņÜ░ļÅä ņĀüņ¦Ć ņĢŖņĢśĻ│Ā ņŗØļÅä ņØ┤ņÖäļČłļŖźņØä ņĀ£ļīĆļĪ£ ņ¦äļŗ©ĒĢśņ¦Ć ļ¬╗ĒĢśļŖö Ļ▓ĮņÜ░ļÅä ņ׳ņŚłļŗż[23]. ņØ┤ļź╝ ĻĘ╣ļ│ĄĒĢśĻĖ░ ņ£äĒĢ┤ 1976ļģä ĒśĖņŻ╝ņØś John DentĻ░Ć Ļ░£ļ░£ĒĢ£ DentsleeveļŖö ĒĢśļČĆņŗØļÅäņĪ░ņ×äĻĘ╝ ņŻ╝ļ│ĆņØś 6 cm ĻĖĖņØ┤ņØś ņä╝ņä£ļź╝ ļ¦īļōżņ¢┤ņä£ ĻĘĖ ņé¼ņØ┤ņŚÉņä£ Ļ░Ćņן ļåÆņØĆ Ļ░ÆņØä ņĖĪņĀĢĒĢśļŖö ļ░®ļ▓ĢņØä ņĀ£ņĢłĒĢśņśĆņ¦Ćļ¦ī ņāüļīĆņĀüņ£╝ļĪ£ ļäÉļ”¼ ņō░ņØ┤ņ¦ĆļŖö ļ¬╗ĒĢśņśĆļŗż[22,24]. ĒĢśņ¦Ćļ¦ī 2000ļģäļīĆļČĆĒä░ ļ»ĖĻĄŁ ņäĖņØĖĒŖĖļŻ©ņØ┤ņŖż ņĪ░ņ¦Ćņøīņŗ▒Ēä┤ ļīĆĒĢÖņØś Ray Clouse ļō▒ņŚÉ ņØśĒĢ┤ņä£ ĻĖ░ņĪ┤ņØś 3~5 cm Ļ░äĻ▓®ņ£╝ļĪ£ ļ░░ņŚ┤ļÉ£ Ļ│ĀņŗØņĀü ļé┤ņĢĢ Ļ▓Ćņé¼ļ▓ĢņØ┤ ņĢäļŗī 1 cm Ļ░äĻ▓®ņ£╝ļĪ£ ņĪ░ļ░ĆĒĢśĻ▓ī ņĢĢļĀź ņä╝ņä£Ļ░Ć ļ░░ņŚ┤ļÉ£ Ļ│ĀĒĢ┤ņāüļÅä ļé┤ņĢĢ Ļ▓Ćņé¼ļ▓ĢņØ┤ ņĪ░ĻĖłņö® ņŚ░ĻĄ¼ ļ¬®ņĀüņ£╝ļĪ£ ņé¼ņÜ®ļÉśĻĖ░ ņŗ£ņ×æĒĢśņśĆļŗż[22,25]. ņØ┤ļ¤¼ĒĢ£ Ļ│ĀĒĢ┤ņāüļÅä ļé┤ņĢĢ Ļ▓Ćņé¼ļ▓ĢņØĆ ĻĖ░ņĪ┤ Ļ│ĀņŗØņĀü ļé┤ņĢĢ Ļ▓Ćņé¼ļ▓ĢņŚÉ ļ╣äĒĢśņŚ¼ Ēø©ņö¼ ļ¦ÄņØĆ ņĀĢļ│┤ļź╝ ņ¢╗ņØä ņłś ņ׳ņŚłņ£╝ļ®░ ņ¦äļŗ©ņŚÉ ņ׳ņ¢┤ņä£ļÅä ĒÜŹĻĖ░ņĀüņØĖ ļ│ĆĒÖöļź╝ Ļ░ĆņĀĖņśżĻ▓ī ļÉśņŚłļŗż(Fig. 1) [25,26]. ļśÉĒĢ£ Ray ClouseļŖö 1 cm Ļ░äĻ▓®ņØś ņä╝ņä£ ņé¼ņØ┤ņØś ņĢĢļĀźĻ░ÆņØä ļŗżņŗ£ 0.1 cm Ļ░äĻ▓®ņØś ņČöņĀĢņ╣ś(interpolation)ļĪ£ ņ▒äņÜ░Ļ│Ā ņØ┤ļź╝ ņĢĢļĀźĻ░ÆņŚÉ ļö░ļźĖ ņ╗¼ļ¤¼ ņØ┤ļ»Ėņ¦Ć(ņĢĢļĀźĻ░ÆņØ┤ ļé«ņ£╝ļ®┤ Ēīīļ×Ćņāē Ļ│äņŚ┤, ņĢĢļĀźĻ░ÆņØ┤ ļåÆņ£╝ļ®┤ ļČēņØĆņāē Ļ│äņŚ┤)ļĪ£ Ēæ£ĒśäĒĢśĻ│Ā ļśÉĒĢ£ ņØ┤ļź╝ ņØ╝ĻĖ░ņśłļ│┤ņŚÉņä£ ņō░ņØ┤ļŹś ļō▒Ļ│ĀņäĀ ņØ┤ļ»Ėņ¦Ćļź╝ ļÅäņ×ģĒĢśņŚ¼ Ēśäņ×¼ ņō░ņØ┤ļŖö Ļ│ĀĒĢ┤ņāüļÅä ļé┤ņĢĢ Ļ▓Ćņé¼ļ▓ĢņØś ĻĖ░ĒŗĆņØä ņ×ĪņĢśļŗż[22,25]. ņØ┤ļĀćĻ▓ī ņ┤śņ┤śĒĢśĻ▓ī ļ░░ņŚ┤ļÉ£ ņĢĢļĀź ņä╝ņä£ļź╝ ĒåĄĒĢśņŚ¼ ļŗżņŗ£ ņČöņĀĢņ╣śĻ╣īņ¦Ć ļŹöĒĢ┤ņĀĖ ņŗØļÅä ļé┤ņØś ņ¢┤ļ¢ż ļČĆņ£äņØś ņĢĢļĀźĻ░ÆļÅä ņĖĪņĀĢņØ┤ Ļ░ĆļŖźĒĢśĻ▓ī ļÉ£ Ļ│ĀĒĢ┤ņāüļÅä ļé┤ņĢĢ Ļ▓Ćņé¼ļŖö ĻĖ░ņĪ┤ņØś Ļ│ĀņŗØņĀü ļé┤ņĢĢ Ļ▓Ćņé¼ņØś Ļ│Āņ¦łņĀüņØĖ ļ¼ĖņĀ£ ņżæ ĒĢśļéśņśĆļŹś ĒĢśļČĆņŗØļÅäņĪ░ņ×äĻĘ╝ņØś Ļ▒░ņ¦ō ņØ┤ņÖäņØä ņóĆ ļŹö ņל ņ░ŠņĢäļé┤Ļ▓ī ļÉśņŚłĻ│Ā, ļśÉĒĢ£ ĻĖ░ņĪ┤ņØś Dentsleeve Ļ░£ļģÉņØä ņĀäĻĖ░ņĀüņØĖ ņŗĀĒśĖ ļČäņäØņØä ĒåĄĒĢśņŚ¼ ļ░£ņĀäņŗ£Ēé© eSleeve Ļ░£ļģÉņØä ļÅäņ×ģĒĢśņśĆļŗż[22]. Ray ClouseļŖö ņé╝Ēé┤ ņØ┤Ēøä 10ņ┤ł ļÅÖņĢłņØś 3ņ┤łĻ░ä Ļ░Ćņן ļé«ņØĆ ĒĢśļČĆņŗØļÅäņĪ░ņ×äĻĘ╝ ļ░öļŗźĻ░ÆņØ┤ Ļ░Ćņן ņ£äņŗØļÅä Ļ▓ĮĻ│äļČĆņØś ņØ┤ņÖäņØä ņל ļ░śņśüĒĢśļŖö ĻĖ░ņżĆĻ░Æņ£╝ļĪ£ ņ▓śņØī ņĀ£ņŗ£ĒĢśņśĆņ£╝ļéś ļÆżņØ┤ņØĆ ņŗ£ņ╣┤Ļ│Ā ĻĘĖļŻ╣ņØś ĒøäņåŹ ņŚ░ĻĄ¼ņŚÉ ļö░ļØ╝ ņé╝Ēé┤ ņØ┤Ēøä 10ņ┤ł ļÅÖņĢłņŚÉ ņ£äņŗØļÅä Ļ▓ĮĻ│äļČĆ ņĢĢļĀźņØś ļ░öļŗźĻ░ÆņØś 4ņ┤ł ņżæņĢÖĻ░ÆņØ┤ ņ£äņŗØļÅä Ļ▓ĮĻ│äļČĆņØś ņØ┤ņÖäņØä Ļ░Ćņן ņל ļ░śņśüĒĢ£ļŗżĻ│Ā ņŚ░ĻĄ¼ Ļ▓░Ļ│╝ļź╝ ļ░£Ēæ£ĒĢśņśĆĻ│Ā, ņØ┤ļź╝ ņĀüļČäļÉ£ ņØ┤ņÖä ņĢĢļĀź(integrated relaxation pressure, IRP)ņ£╝ļĪ£ ņĀĢņØśĒĢśņŚ¼ Ēśäņ×¼ ņé¼ņÜ®ĒĢśļŖö ņŗ£ņ╣┤Ļ│Ā ĻĖ░ņżĆņØś ĻĖ░ņżĆņĀÉņØ┤ ļÉśņŚłļŗż(Fig. 2) [22,27]. ĒĢ£ĒÄĖ, ņŗ£ņ╣┤Ļ│Ā ļģĖņŖżņø©ņŖżĒä┤ļīĆĒĢÖņØś John PandolfinoļŖö Ļ│ĀĒĢ┤ņāüļÅä ļé┤ņĢĢ Ļ▓Ćņé¼ Ļ▓░Ļ│╝Ļ░ÆņØä ļ░öĒāĢņ£╝ļĪ£ ĒĢ£ ņŗØļÅä ņØ┤ņÖäļČłļŖź ĒÖśņ×ÉļōżņØś ļé┤ņĢĢĻ▓Ćņé¼ ĻĘĖļ”╝ņØä Ļ┤Ćņ░░ĒĢśļŹś ņżæ, 3Ļ░£ņØś ņĢäĒśĢņØ┤ ņĪ┤ņ×¼ĒĢ£ļŗżļŖö Ļ▓āņØä ļ░£Ļ▓¼ĒĢśņśĆĻ│Ā ņØ┤ļ¤░ 3Ļ░£ņØś ņĢäĒśĢņŚÉ ļö░ļØ╝ ņ╣śļŻī Ēøä ņśłĒøäĻ░Ć ļŗżļź┤ļŗżļŖö Ļ▓āļÅä ļ░£Ēæ£ĒĢśņśĆļŗż[28]. PandolfinoņŚÉ ņØśĒĢśļ®┤ IRP ņłśņ╣śļŖö ļ╣äņĀĢņāüņĀüņ£╝ļĪ£ ļåÆņ£╝ļéś ņŗØļÅä ņ▓┤ļČĆņÜ┤ļÅÖņØ┤ ņĀäĒśĆ Ļ┤Ćņ░░ļÉśņ¦Ć ņĢŖļŖö 1ĒśĢ, ņŗØļÅä ņ▓┤ļČĆņØś ļÅīļ”╝ĻĘ╝ņ£ĪņĖĄ(circular muscle layer)ņØś ņÜ┤ļÅÖņØĆ ļ¢©ņ¢┤ņĀĖ ņ׳ņ£╝ļéś ņäĖļĪ£ĻĘ╝ņ£ĪņĖĄ(longitudinal muscle layer)ņØś ņÜ┤ļÅÖļ¦ī ņØ╝ļČĆ ļé©ņĢäņä£ ņĀäņŗØļÅä Ļ░ĆņĢĢņØ┤ 20% ņØ┤ņāüņØś ņé╝Ēé┤ņŚÉņä£ Ļ┤Ćņ░░ļÉśļŖö 2ĒśĢ, ĒĢśļČĆņŗØļÅä ņ▓┤ļČĆņØś ņłśņČĢņØä 20% ņØ┤ņāüņØś ņé╝Ēé┤ņŚÉņä£ Ļ┤Ćņ░░ļÉśļŖö 3ĒśĢņ£╝ļĪ£ ņāłļĪŁĻ▓ī ĻĄ¼ļČäĒĢśņśĆĻ│Ā(Fig. 2), ĒŖ╣Ē׳ 2ĒśĢņØś Ļ▓ĮņÜ░ ņ╣śļŻī ņØ┤Ēøä ņ”Øņāü Ļ░£ņäĀņØ┤ ļŗżļźĖ 1ĒśĢņØ┤ļéś 3ĒśĢņŚÉ ļ╣äĒĢ┤ņä£ ņ£ĀņØśĒĢśĻ▓ī ļåÆļŗżļŖö Ļ▓āņØ┤ ņŚ¼ļ¤¼ ņŚ░ĻĄ¼ļź╝ ĒåĄĒĢśņŚ¼ ņĢīļĀżņĪīļŗż[1,28,29]. ņØ┤ļ¤¼ĒĢ£ 3Ļ░£ņØś ņĢäĒśĢņØś ļČäļźśļŖö 2021ļģäņŚÉ ļ░£Ēæ£ļÉ£ ņŗ£ņ╣┤Ļ│Ā 4ļ▓łņ¦Ė Ļ░£ņĀĢĒīÉĻ╣īņ¦Ć ņØ┤ņ¢┤ņ¦ĆĻ│Ā ņ׳ļŗż(Table 1) [4]. ĒĢśņ¦Ćļ¦ī ņŚ¼ļ¤¼ ņŚ░ĻĄ¼ Ļ▓░Ļ│╝ļōżņØä ĒåĄĒĢśņŚ¼ ņĀüļČäļÉ£ ņØ┤ņÖä ņĢĢļĀźĻ░ÆņØ┤ ņĀĢņāüņ×äņŚÉļÅä ļČłĻĄ¼ĒĢśĻ│Ā ņŗØļÅä ņØ┤ņÖäļČłļŖźņØĖ Ļ▓ĮņÜ░ļÅä ļ░ØĒśĆņ¦Ćļ®┤ņä£ ņāłļĪŁĻ▓ī Ļ░£ņĀĢļÉ£ ņŗ£ņ╣┤Ļ│Ā 4ļ▓łņ¦Ė Ļ░£ņĀĢĒīÉņŚÉņä£ļŖö ĒøäņłĀĒĢĀ ņŚ¼ļ¤¼ Ļ░Ćņ¦Ć ņČöĻ░ĆņĀüņØĖ ļ░®ļ▓ĢņØä ĒåĄĒĢśņŚ¼ ĒÖĢņ¦äņØä ĻČīņןĒĢśĻ│Ā ņ׳ļŗż[30]. ļśÉĒĢ£, ņŗØļÅäļé┤ņĢĢ Ļ▓Ćņé¼ ĒöäļĪ£ĒåĀņĮ£ņŚÉņä£ļÅä ņČöĻ░ĆņĀüņ£╝ļĪ£ ļ│ĆĒÖöļź╝ ņŻ╝ņ¢┤ņä£ ĻĖ░ņĪ┤ņŚÉ ļŗ©ņł£ĒĢśĻ▓ī ļłäņÜ┤ ņ×ÉņäĖņŚÉņä£ 10ļ▓łņØś ņé╝Ēé┤ņØä ĒåĄĒĢśņŚ¼ ņ¦äļŗ©ĒĢśļŖö Ļ▓ā ņÖĖņŚÉ ņŚ¼ļ¤¼ Ļ░Ćņ¦Ć ņČöĻ░ĆņĀüņØĖ Ļ▓Ćņé¼ļōżņØä ĻČīņןĒĢśĻ│Ā ņ׳ļŗż[4]. ņ”ē, ļłäņÜ┤ ņ×ÉņäĖņŚÉņä£ 2~3ņ┤ł Ļ░äĻ▓®ņ£╝ļĪ£ 2 mL ņŗØņŚ╝ņłśļź╝ 5ĒÜī ņé╝ĒéżĻ▓ī ĒĢśļŖö ļŗżņżæĻĖēņåŹņé╝Ēé┤ Ļ▓Ćņé¼(multiple rapid swallow test)ļź╝ ņŗ£Ē¢ēĒĢśļ®░, ņØ┤ļź╝ ĒåĄĒĢśņŚ¼ ņŗØļÅä ņ▓┤ļČĆņØś ņłśņČĢ ņŚ¼ļĀź(contractile reserve)ņØä ņĢīņĢäļ│╝ ņłś ņ׳ļŗżĻ│Ā ņĢīļĀżņĪīļŗż[4,31]. ĻĘĖ Ēøä ņ▓┤ņ£äļź╝ ļ░öĻ┐öņä£ ņĢēņØĆ ņ×ÉņäĖņŚÉņä£ ļŗżņŗ£ ņŗØņŚ╝ņłśļź╝ 5ĒÜī ņé╝ĒéżĻ▓ī ĒĢśļŖöļŹ░, Ļ▓Ćņé¼ ļÅäņżæņŚÉ ņ×ÉņäĖļź╝ ļ░öĻŠĖļŖö ņØ┤ņ£ĀļŖö ņ£äņŗØļÅä ņĀæĒĢ®ļČĆ ņČ£ĻĄ¼ ĒÅÉņćä(esophagogastric junction outflow obstruction) Ļ░ÖņØĆ Ļ▓ĮņÜ░ ņ╣┤ĒģīĒä░ņŚÉ ņĀĢņāüņĀüņØĖ ņŗØļÅä ļé┤Ļ░Ģ ļé┤ņØś ĻĄ¼ņĪ░ļ¼╝ ļō▒ņØ┤ ļŗ┐ņĢäņä£ ņĀüļČäļÉ£ ņØ┤ņÖä ņĢĢļĀźĻ░ÆņØ┤ ļ╣äņĀĢņāüņĀüņ£╝ļĪ£ ļåÆĻ▓ī ļéśņśżļŖö Ļ▓āņØä ļ░░ņĀ£ĒĢśĻĖ░ ņ£äĒĢ┤ņä£ ļō▒ņØś ņØ┤ņ£ĀņØ┤ļŗż[4,32]. ļŗżņØīņ£╝ļĪ£ļŖö 200 mLņØś ļ¼╝ņØä ņĄ£ļīĆĒĢ£ ņŚ░ļŗ¼ņĢäņä£ ņé╝ĒéżĻ▓ī ĒĢśļŖö ĻĖēņåŹņé╝Ēé┤ Ļ▓Ćņé¼(rapid drink challenge)ļź╝ ņ¦äĒ¢ēĒĢśĻ▓ī ļÉśļŖöļŹ░ ņØ┤ļź╝ ĒåĄĒĢśņŚ¼ ņ£äņŗØļÅä Ļ▓ĮĻ│äļČĆ(esophagogastric junction)ņØś ĻĖ░ļŖźņØä ĒīīņĢģĒĢśļŖö ļŹ░ ļÅäņøĆņØ┤ ļÉ£ļŗżĻ│Ā ĒĢśļ®░, ĒŖ╣Ē׳ ņĀüļČäļÉ£ ņØ┤ņÖä ņĢĢļĀź ņłśņ╣śĻ░Ć ļé«Ļ▒░ļéś ņĢĀļ¦żĒĢ£ Ļ▓ĮņÜ░ņŚÉņä£ ĻĖēņåŹņé╝Ēé┤ Ļ▓Ćņé¼ļź╝ ņŗ£Ē¢ēĒĢśņŚ¼ ņŗØļÅä ņØ┤ņÖäļČłļŖź ļō▒ņØś ņ¦äļŗ©ņŚÉ ļÅäņøĆņØ┤ ļÉ£ļŗżĻ│Ā ĒĢ£ļŗż[4,31,33]. ĻĘĖ ņÖĖ ļ░ź Ļ░ÖņØĆ Ļ│ĀĒśĢ ņŗØņØ┤ļź╝ ļ©╣ņØ┤Ļ▒░ļéś amyl nitrate ļō▒ņØś ņĢĮļ¼╝ Ēł¼ņŚ¼ ļō▒ņØä ĒåĄĒĢśņŚ¼ ņ£Āļ░£ Ļ▓Ćņé¼ļź╝ ņČöĻ░ĆņĀüņ£╝ļĪ£ ņŗ£Ē¢ēĒĢĀ ņłśļÅä ņ׳ļŗż[4]. ļ¦īņĢĮ ņØ┤ļ¤¼ĒĢ£ Ļ▓Ćņé¼ļź╝ ņ¦äĒ¢ēĒ¢łņØīņŚÉļÅä ņØ┤ņāü ņåīĻ▓¼ņØ┤ ļ¬ģĒÖĢĒĢśņ¦Ć ņĢŖĻ▒░ļéś ņ¦äļŗ©ņØ┤ ņĢĀļ¦żĒĢ£ Ļ▓ĮņÜ░ņŚÉ ļīĆĒĢ┤ņä£ ņŗ£ņ╣┤Ļ│Ā 4ĒīÉ Ļ░£ņĀĢĒīÉņŚÉņä£ļŖö Ēöīļ”Į(functional lumen imaging probe, FLIP)Ļ│╝ ņŗ£Ļ░äņ░© ļ░öļź© ņŗØļÅäņĪ░ņśüņłĀ(timed barium esophagogram) ļō▒ņØś Ļ▓Ćņé¼ļź╝ ļ│┤ņĪ░ņĀüņØĖ ņ¦äļŗ© ļÅäĻĄ¼ļĪ£ņä£ņØś ņŚŁĒĢĀņØä ņØĖņĀĢĒĢśļ®┤ņä£ ņØ┤ļ¤¼ĒĢ£ ĒĢ£Ļ│äļź╝ ĻĘ╣ļ│ĄĒĢśĻ│Āņ×É ĒĢśņśĆļŗż[2,4]. Ēöīļ”ĮņŚÉņä£ļŖö ņ£äņŗØļÅä ņĀæĒĢ®ļČĆ-Ēāäņä▒ļÅä(esophagogastric junction-distensibility index)Ļ░Ć 3.0 ņØ┤ĒĢśņØ┤ļ®┤ņä£ ļ╣äņĀĢņāüņĀüņØĖ ņłśņČĢņØä ļ│┤ņØ╝ ļĢī ĻĘĖļ”¼Ļ│Ā ņŗ£Ļ░äņ░© ļ░öļź© ņĪ░ņśüņłĀņŚÉņä£ļŖö 5ļČä ņØ┤ņāü ļ░öļź©ņØ┤ 5 cm ņØ┤ņāü ļ©Ėļ¼╝ļ¤¼ ņ׳Ļ▒░ļéś 1ļČä ņØ┤ņāü ĒāĆļĖöļĀøņØ┤ ļ©Ėļ¼╝ļ¤¼ ņ׳ņØä ļĢīļĪ£ ļ╣äņĀĢņāüņØä ņĀĢņØśĒĢśņśĆļŗż[2,4].
ņ×äĒö╝ļŹśņŖż ļ®┤ņĀü ņĖĪņĀĢ(impedance planimetry)ņØä ņØ┤ņÜ®ĒĢ£ ņŗØļÅä ĻĖ░ļŖź ņŚ░ĻĄ¼ļŖö 1990ļģäļīĆļČĆĒä░ ņŗżĒŚśņĀüņ£╝ļĪ£ ņØ┤ļŻ©ņ¢┤ņĀĖ ņÖöņ£╝ļ®░, ņŗżņĀ£ ņ×äņāüņŚÉņä£ ĻĘĖ ņØ┤ņÜ®ņØ┤ Ļ░ĆļŖźĒĢ┤ņ¦ä Ļ▓āņØĆ Hans Gregersen ļō▒ņŚÉ ņØśĒĢ┤ņä£ FLIP (endoFLIP; Medtronic, Minneapolis, MN, USA)ņØ┤ļØ╝ļŖö ĒśĢĒā£ļĪ£ ļ░£ņĀäļÉ£ ņØ┤ĒøäņØ┤ļŗż[34,35]. ņØ┤ļź╝ ņāüņÜ®ĒÖöĒĢ£ Ļ▓āņØ┤ endoFLIPņØ┤ļ®░, ņØ┤ļź╝ ņ×äņāüņŚÉņä£ ĒÖ£ņÜ®ĒĢ£ ņŚ░ĻĄ¼ļŖö 2010ļģäļīĆ ņ┤łļ░śļČĆĒä░ ņŗ£ņ╣┤Ļ│Ā ļģĖņŖżņø©ņŖżĒä┤ ĻĘĖļŻ╣ņŚÉņä£ ņŗ£ņ×æĒĢśņśĆļŗż[36-38]. ĒŖ╣Ē׳, endoFLIPņŚÉņä£ļŖö ņ×äĒö╝ļŹśņŖż ļ®┤ņĀü ņĖĪņĀĢņØä ļ░öĒāĢņ£╝ļĪ£ ļé┤Ļ░ĢņØś ļŗ©ļ®┤ņĀü ļ░Å ņĢĢļĀźņØä ņĖĪņĀĢĒĢĀ ņłś ņ׳Ļ│Ā, ņØ┤ļź╝ ļ░öĒāĢņ£╝ļĪ£ ĒĢśņŚ¼ ļé┤Ļ░Ģ ļśÉļŖö ņĪ░ņ×äĻĘ╝ņØś ĒīĮņ░ĮļŖźņØä ņĖĪņĀĢĒĢĀ ņłś ņ׳ļŗż[37-39].
ņŗØļÅä ņØ┤ņÖäļČłļŖźņØś ļ│æĒā£ņāØļ”¼ļź╝ ņāØĻ░üĒĢ┤ļ│┤ļ®┤, ņĢĀņ┤łņŚÉ ĒĢśļČĆņŗØļÅäņĪ░ņ×äĻĘ╝ņØś ļČłņÖäņĀäĒĢ£ ņØ┤ņÖäņŚÉ ņØśĒĢ┤ ļ░£ņāØĒĢśļŖö ļ│æņØ┤ļ»ĆļĪ£ 5 mLņö®ņØś ņŚŁļÅÖņĀüņØĖ ņé╝Ēé┤ņØ┤ ņŚåņ£╝ļ®┤ ņĢäļ¼┤ ņŗĀĒśĖļÅä ņ▓┤Ēü¼ļÉśņ¦Ć ņĢŖņĢäņä£ ņāüļīĆņĀüņ£╝ļĪ£ ņŚŁļÅÖņĀüņØĖ ļé┤ļČĆļĪ£ņØś ņłśņČĢļĀźņØä ĒÅēĻ░ĆĒĢśļŖö ņŗØļÅäļé┤ņĢĢ Ļ▓Ćņé¼ļ│┤ļŗżļŖö ņāüļīĆņĀüņ£╝ļĪ£ ņłśļÅÖņĀüņØĖ ņŗØļÅä ļ░öĻ╣źņ£╝ļĪ£ņØś ņŗØļÅäņĪ░ņ×äĻĘ╝ņØś ĒīĮņ░ĮļŖźņØä ĒÅēĻ░ĆĒĢĀ ņłś ņ׳ļŖö Ēöīļ”Į Ļ░ÖņØĆ Ļ▓Ćņé¼Ļ░Ć ņśżĒ׳ļĀż ļŹö ņĀĢĒÖĢĒĢĀ ņłśļÅä ņ׳ļŗżĻ│Ā ņØ╝ļČĆ ņŚ░ĻĄ¼ņŚÉņä£ ņŻ╝ņןļÉśĻ│Ā ņ׳ļŗż[40,41].
ĒØöĒ׳ ņŗØļÅäņŚÉņä£ ņō░ņØ┤ļŖö Ēöīļ”Į ņ╣┤ĒģīĒä░ļŖö 8 cm (16Ļ░£ņØś ņ×äĒö╝ļŹśņŖż ņä╝ņä£Ļ░Ć 0.5 cm Ļ░äĻ▓® ļ░░ņŚ┤)ņÖĆ 16 cm (16Ļ░£ņØś ņ×äĒö╝ļŹśņŖż ņä╝ņä£Ļ░Ć 1 cm Ļ░äĻ▓® ļ░░ņŚ┤) ļæÉ ņóģļźśĻ░Ć ņ׳ļŖöļŹ░, 8 cm ņ╣┤ĒģīĒä░ļŖö ņ£äņŗØļÅä Ļ▓ĮĻ│äļČĆņØś ĒīĮņ░ĮļŖźĻ│╝ ļŗ©ļ®┤ņĀü ņĖĪņĀĢņØ┤ Ļ░ĆļŖźĒĢśĻ│Ā, 16 cm ņ╣┤ĒģīĒä░ļŖö ĻĘĖ ņÖĖ ņČöĻ░ĆņĀüņ£╝ļĪ£ ņŗØļÅäļé┤Ļ░ĢņØś 2ņ░© ņŚ░ļÅÖņÜ┤ļÅÖļÅä ĒīīņĢģņØ┤ Ļ░ĆļŖźĒĢśļŗż[41]. ļśÉĒĢ£ ņĄ£ĻĘ╝ņŚÉ Ēöīļ”ĮņØä ņØ┤ņÜ®ĒĢśņŚ¼ 2ņ░© ņŚ░ļÅÖņÜ┤ļÅÖņØś ĒīīĒśĢņØä ļČäņäØĒĢ£ panometryņŚÉņä£ļŖö ņé╝Ēé┤Ļ│żļ×Ćņ£╝ļĪ£ ļé┤ņøÉĒĢ£ ĒÖśņ×Éļōż ņżæņŚÉņä£ Ļ│ĀĒĢ┤ņāüļÅä ļé┤ņĢĢ Ļ▓Ćņé¼ņŚÉņä£ ņĀĢņāüņØ┤ņŚłļŹś ĒÖśņ×ÉņØś 50%ņŚÉņä£ ļ╣äņĀĢņāü Ēöīļ”Į ņåīĻ▓¼ņØä ļ│┤ņŚ¼ņä£ ņ¦äļŗ©ņØ┤ Ļ░ĆļŖźĒ¢łļŗżļŖö ņŚ░ĻĄ¼ Ļ▓░Ļ│╝ļÅä ņ׳ļŗż[41-43]. ņĄ£ĻĘ╝ ņŚ░ĻĄ¼ļōżņØä ņóģĒĢ®ĒĢśļ®┤ ĒīĮņ░ĮļŖźņØä ĻĖ░ņżĆņ£╝ļĪ£ 2 mm2/mmHg ņØ┤ĒĢśļØ╝ļ®┤ ļ╣äņĀĢņāüņ£╝ļĪ£ Ļ░äņŻ╝ļÉśļ®░, 2~3 mm2/mmHg ņé¼ņØ┤ļŖö Ļ▓ĮĻ│äļČĆ, 3 mm2/mmHg ņØ┤ņāüņØĆ ņĀĢņāüņ£╝ļĪ£ ņŚ¼Ļ▓©ņ¦äļŗż[41]. ļśÉĒĢ£, ņŗØļÅä ņØ┤ņÖäļČłļŖź ĒÖśņ×É ņżæņŚÉņä£ļÅä ņĢ× ļ░®Ē¢ź 2ņ░© ņŚ░ļÅÖņÜ┤ļÅÖ ļō▒ņØ┤ ņØ╝ļČĆ ņé┤ņĢäņ׳ļŖö Ļ▓ĮņÜ░ņŚÉļŖö Ļ▓ĮĻĄ¼ņĀü ļé┤ņŗ£Ļ▓ĮņĀü ĻĘ╝ņĀłĻ░£ņłĀ ļō▒ ņŗ£ņłĀ ņØ┤Ēøä ņŗØļÅä ņ▓┤ļČĆ ņÜ┤ļÅÖļŖźņØ┤ ņØ╝ļČĆ ĒÜīļ│ĄļÉśĻ▒░ļéś ņ”Øņāü Ļ░£ņäĀņØś ņŚ¼ņ¦ĆĻ░Ć ņóĆ ļŹö ņ׳ņØä Ļ▓āņ£╝ļĪ£ ņśłņĖĪĒĢśļŖö ņØ╝ļČĆ ņåīĻĘ£ļ¬© ņŚ░ĻĄ¼Ļ░Ć ņ׳ņ£╝ļéś, ņØ┤ņŚÉ ļīĆĒĢ┤ņä£ļŖö ļīĆĻĘ£ļ¬©ņØś ņĀäĒ¢źņĀü ņŚ░ĻĄ¼Ļ░Ć ĒĢäņÜöĒĢĀ Ļ▓āņ£╝ļĪ£ ļ│┤ņØĖļŗż[41,43].
ņŗ£Ļ░äņ░© ļ░öļź© ņĪ░ņśüņłĀņØĆ 100~200 mLņØś ņĀĆļ░ĆļÅä ļ░öļź©ņØä ņäĀ ņ×ÉņäĖņŚÉņä£ ļ¦łņŗ£Ļ│Ā, 1ļČä, 2ļČä, 5ļČä Ēøä Ļ░üĻ░ü ņŗØļÅäņØś ņŚæņŖżņäĀ ņé¼ņ¦äņØä ņ¢╗ņ¢┤ņä£ ļ░öļź©ņØś ņĀĆļźśļź╝ ĒÖĢņØĖĒĢśļŖö ļ░®ļ▓ĢņØ┤ļ®░, ņŗØļÅäļé┤ņĢĢ Ļ▓Ćņé¼ņØś ļ│┤ņĪ░ņĀüņØĖ ņ¦äļŗ© Ļ▓Ćņé¼ļĪ£ņä£ ļÅäņøĆņØ┤ ļÉĀ ņłś ņ׳ļŗż[5]. ņĄ£ĻĘ╝ ņŚ¼ļ¤¼ ņŚ░ĻĄ¼ņŚÉņä£ ņŗ£Ļ░äņ░© ļ░öļź© ņĪ░ņśüņłĀņØ┤ ņŗØļÅä ņØ┤ņÖäļČłļŖźņØś ņ¦äļŗ© ļ░Å ņśłĒøä ĒīÉņĀĢņŚÉ ļÅäņøĆņØ┤ ļÉ£ļŗżĻ│Ā ļ│┤Ļ│ĀĒĢśņśĆļŗż[5]. ņŗØļÅä ņØ┤ņÖäļČłļŖź ĒÖśņ×ÉļōżņØä ļīĆņāüņ£╝ļĪ£ ĒĢ£ ļīĆĻĘ£ļ¬© ņŚ░ĻĄ¼ņŚÉ ņØśĒĢśļ®┤ ļ░öļź©ņØä ņé╝Ēé© Ēøä 1ļČä ļÆż ļ░öļź© ņøÉņŻ╝ ļåÆņØ┤Ļ░Ć 5 cm ņØ┤ņāü ļé©ņĢä ņ׳ņØä ļĢī 94% ļ»╝Ļ░ÉļÅäņÖĆ 71% ĒŖ╣ņØ┤ļÅäļź╝ ļ│┤Ļ│ĀĒĢśņśĆĻ│Ā, 13 mm ņ¦Ćļ”äņØś ļ░öļź© ĒāĆļĖöļĀøņØ┤ ļ╣ĀņĀĖļéśĻ░Ćņ¦Ć ļ¬╗ĒĢśĻ│Ā ņ£äņŗØļÅä Ļ▓ĮĻ│äļČĆņŚÉ Ļ▒Ėļ”¼ļŖö Ļ▓āņØ┤ ņ¦äļŗ©ņŚÉ ļÅäņøĆņØ┤ ļÉ©ņØä ļ│┤Ļ│ĀĒĢśņśĆļŗż[44].
ņĀä ņäĖĻ│äņĀüņ£╝ļĪ£ ļ¦łņĢĮļźś ņ¦äĒåĄņĀ£ ļō▒ņØś ņé¼ņÜ® ņ”ØĻ░ĆņŚÉ ļö░ļØ╝ ļ¦łņĢĮņä▒ ņĢĮņĀ£ņŚÉ ņØśĒĢ£ ņŗØļÅäņÜ┤ļÅÖ ņØ┤ņāüļÅä ņĢīļĀżņ¦ĆĻ│Ā ņ׳ļŖöļŹ░, ļ¦łņĢĮņä▒ ņ¦äĒåĄņĀ£ļź╝ ņןĻĖ░Ļ░ä ļ│ĄņÜ®ĒĢśļ®┤ ĒĢśļČĆņŗØļÅäņĪ░ņ×äĻĘ╝ņØś ņØ┤ņÖäņØ┤ ļ¢©ņ¢┤ņ¦Ćļ®░ ĒĢśļČĆņŗØļÅä ņ▓┤ļČĆņØś ņĢĢļĀź ļ░Å ņåŹļÅäĻ░Ć ņ”ØĻ░ĆĒĢśļ®┤ņä£ ņŗØļÅä ņ▓┤ļČĆņØś ļÅÖņŗ£ņä▒ ņłśņČĢņØä ļ│┤ņØ┤Ļ│Ā ņ£äņŗØļÅä Ļ▓ĮĻ│äļČĆņØś ņĢĢļĀźņØ┤ ņ”ØĻ░ĆĒĢśĻ▓ī ļÉśļ®┤ņä£ ļ¦łņ╣ś ņŗØļÅä ņØ┤ņÖäļČłļŖźņ”Ø 3ĒśĢņ▓śļ¤╝ ļ│┤ņØ┤Ļ▓ī ļÉ£ļŗż[32,45-47]. ņØ┤ļ¤░ ĒÖśņ×ÉļōżņŚÉņä£ ĒĢ┤ļŗ╣ ņĢĮņĀ£ļź╝ ņżæļŗ©ĒĢśļ®┤ ņØ┤ļ¤¼ĒĢ£ ņØ┤ņāü ņåīĻ▓¼ņØ┤ ņØ╝ļČĆ ĒśĖņĀäļÉśĻ│Ā ņé╝Ēé┤Ļ│żļ×Ć ļō▒ņØś ņ”ØņāüļÅä ĒśĖņĀäļÉśļŖö Ļ▓āņØ┤ ļ¦łņĢĮņä▒ ņŗØļÅä ĻĖ░ļŖź ņØ┤ņāüņØś ĒŖ╣ņ¦ĢņØ┤ļØ╝Ļ│Ā ĒĢĀ ņłś ņ׳ļŗż[32,45]. ļö░ļØ╝ņä£, ņŗØļÅäļé┤ņĢĢ Ļ▓Ćņé¼ ņĀäņŚÉ ĒÅēņåī ļ│ĄņÜ®ĒĢśĻ│Ā ņ׳ļŹś ņĢĮņĀ£ņŚÉ ļīĆĒĢ┤ņä£ļÅä ņ×ÉņäĖĒĢśĻ▓ī ĒÖĢņØĖĒĢśļŖö Ļ▓āņØ┤ ņżæņÜöĒĢśļŗż[32,45].
ļśÉĒĢ£, ĒĢśļČĆņŗØļÅäļéś ņ£äņŗØļÅä Ļ▓ĮĻ│äļČĆņŚÉ ļ░£ņāØĒĢ£ ņĢöņØ┤ļéś ĒÅÉņĢö ņżæņŚÉņä£ļÅä ņåīņäĖĒżņĢöņØś Ļ▓ĮņÜ░ ņóģņóģ ņŗØļÅä ņØ┤ņÖäļČłļŖźņ”ØĻ│╝ ņ£Āņé¼ĒĢ£ ĒśĢĒā£ļĪ£ ļ░£ĒśäĒĢśĻĖ░ ļĢīļ¼ĖņŚÉ ņ¦äļŗ©ņŚÉ ņ׳ņ¢┤ ņŻ╝ņØśļź╝ ņÜöĒĢ£ļŗż[5]. ļ¦īņĢĮ 1ļģä ņØ┤ĒĢśņØś ņ¦¦ņØĆ ĻĖ░Ļ░ä ļé┤ņŚÉ ņé╝Ēé┤Ļ│żļ×ĆņØ┤ ņāØĻ▓╝Ļ▒░ļéś, ņ▓┤ņżæ Ļ░ÉņåīĻ░Ć ņ׳ņ£╝ļ®┤ņä£ Ļ│ĀļĀ╣ņØś ĒÖśņ×ÉņØĖ Ļ▓ĮņÜ░ņŚÉļŖö CT ļō▒ņØś Ļ▓Ćņé¼ļź╝ ĒåĄĒĢśņŚ¼ 2ņ░©ņĀüņØĖ ņŗØļÅä ņØ┤ņÖäļČłļŖź Ļ░ĆļŖźņä▒ņØä Ļ░Éļ│äĒĢśļŖö Ļ▓āņØ┤ ĒĢäņÜöĒĢśļŗż.5 Ļ░äĒś╣ ĒÅÉņĢö ņżæņŚÉņä£ļÅä ņåīņäĖĒżņĢöņØś Ļ▓ĮņÜ░ņŚÉ ņŗĀņāØļ¼╝ļöĖļ”╝ ņ”ØĒøäĻĄ░(paraneoplastic syndrome)ņØś ņ”Øņāüņ£╝ļĪ£ 2ņ░©ņĀüņØĖ ņŗØļÅä ņØ┤ņÖäļČłļŖźņØä ļ│┤ņØ╝ ņłś ņ׳Ļ│Ā, ņØ┤ļ¤░ Ļ▓ĮņÜ░ antineuronal nuclear antibody (anti-ANNA) 1 & 2, aka anti-Hu antibody ļō▒ņØś Ļ▓Ćņé¼Ļ░Ć ļÅäņøĆņØ┤ ļÉĀ ņłśļÅä ņ׳ļŗż[5].
ņ╣╝ņŖśĒåĄļĪ£ ņ░©ļŗ©ņĀ£, ņ¦łņé░ņŚ╝ņĀ£ņ×¼, ĒĢŁņĮ£ļ”░ņĢĮņĀ£, ĒżņŖżĒżļŗżņØ┤ņŚÉņŖżĒä░ļČäĒĢ┤ĒÜ©ņåī(phosphodiesterase) ļō▒ņØś ņĢĮņĀ£Ļ░Ć ņō░ņØ╝ ņłś ņ׳ļŗż. ĒĢśņ¦Ćļ¦ī ņØ┤ļ¤░ ņĢĮņĀ£Ļ░Ć ĒĢśļČĆņŗØļÅäņĪ░ņ×äĻĘ╝ ņĢĢļĀźņØä ņØ╝ņŗ£ņĀüņ£╝ļĪ£ ļ¢©ņ¢┤ļ£©ļ”¼ļŖö ĒÜ©Ļ│╝ļŖö ņ׳ļŹöļØ╝ļÅä ļ╣äĻĄÉņĀü ņ¦¦ņØĆ ņ¦ĆņåŹņŗ£Ļ░ä ļĢīļ¼ĖņŚÉ ņŚ¼ļ¤¼ ļ▓ł ļ░śļ│Ą Ēł¼ņŚ¼ļź╝ ņÜöĒĢśļŗż ļ│┤ļŗł, ļæÉĒåĄ, ņĀĆĒśłņĢĢ, ļČĆņóģ ļō▒ņØś ļČĆņ×æņÜ®ņØ┤ ņĀüņ¦Ć ņĢŖĻ▓ī ļ│┤Ļ│ĀļÉ£ļŗż. ļö░ļØ╝ņä£ ĒøäņłĀĒĢĀ ļé┤ņŗ£Ļ▓Į ņŗ£ņłĀņØ┤ļéś ņłśņłĀņĀüņØĖ ņ╣śļŻīļź╝ ļ¬╗ĒĢśļŖö ņØ╝ļČĆ ĒÖśņ×ÉļōżņŚÉņä£ Ļ│ĀļĀżĒĢĀ ņłś ņ׳ļŗż[5,19,21].
ļé┤ņŗ£Ļ▓ĮņØä ĒåĄĒĢśņŚ¼ ļ│┤ĒŖżļ”¼ļŖä ļÅģņåīļź╝ ņŻ╝ņé¼ĒĢśņŚ¼ ĒĢśļČĆņŗØļÅä ļ░Å ĒĢśļČĆņŗØļÅäņĪ░ņ×äĻĘ╝ņØś ņĮ£ļ”░ņä▒ ņ×ÉĻĘ╣ņØä ļ¦ēņĢäņä£ ĻĘ╝ņ£ĪņØś ņØ╝ņŗ£ņĀüņØĖ ļ¦łļ╣äļź╝ ņØ╝ņ£╝ņ╝£ņä£ ņ”Øņāü Ļ░£ņäĀņØä ļģĖļ”¼ļŖö ņ╣śļŻīļĪ£ņä£, ļīĆĻ░£ 100 UņØś ļ│┤ĒŖżļ”¼ļŖä ļÅģņåīļź╝ ņŻ╝ņé¼ĒĢśĻ▓ī ļÉ£ļŗż. ļČĆņ×æņÜ®ņØĆ ļ¦żņÜ░ ļé«ļŗżĻ│Ā ņĢīļĀżņĀĖ ņ׳ņ£╝ļ®░, 315ļ¬ģņØä ļīĆņāüņ£╝ļĪ£ ĒĢ£ 9Ļ░£ņØś ņŚ░ĻĄ¼ļź╝ ņóģĒĢ®ĒĢ£ ļ®öĒāĆļČäņäØņŚÉ ņØśĒĢśļ®┤ ņŗ£ņłĀ 30ņØ╝ ņØ┤ļé┤ņØś ņ”Øņāü Ļ░£ņäĀņ£©ņØ┤ 78% ņĀĢļÅäļĪ£ ņĢīļĀżņĀĖ ņ׳ļŗż[5,21,48]. ĒĢśņ¦Ćļ¦ī ņ¦ĆņåŹļĀźņØĆ ļ¢©ņ¢┤ņĀĖņä£ 12Ļ░£ņøöņØ┤ ņ¦Ćļéśļ®┤ 40% ņĀĢļÅäļ¦ī ņ”Øņāü ĒśĖņĀäņØä ņ£Āņ¦ĆĒĢ£ļŗżĻ│Ā ĒĢśļ®░ Ļ▓░ĻĄŁ ņČöĻ░ĆņĀüņØĖ ļ│┤ĒŖżļ”¼ļŖä ņŻ╝ņé¼ ņ╣śļŻīļéś ĻĖ░ĒāĆ ļé┤ņŗ£Ļ▓ĮņĀü ņ╣śļŻī ļō▒ņØ┤ ĒĢäņÜöĒĢśĻ▓ī ļÉśļ»ĆļĪ£ ļé┤ņŗ£Ļ▓Į ņ╣śļŻī ļō▒ņØ┤ ņēĮņ¦Ć ņĢŖņØĆ Ļ│ĀļĀ╣ņØś ĒÖśņ×ÉņŚÉņä£ ņØ╝ņŗ£ņĀüņØĖ ņ”Øņāü Ļ░£ņäĀņØä ļģĖļ”¼Ļ│Ā ņŗ£ļÅäĒĢ┤ ļ│╝ ņłś ņ׳ņØä Ļ▓āņ£╝ļĪ£ ņāØĻ░üļÉ£ļŗż[5,21].
ĒÆŹņäĀņØä ĒĢśļČĆņŗØļÅäņĪ░ņ×äĻĘ╝ ņŻ╝ļ│Ćņ£╝ļĪ£ ņéĮņ×ģĒĢśņŚ¼ ĒÖĢņןņŗ£ĒéżļŖö ņŗ£ņłĀļĪ£ņä£, 30, 35, 40 mm ņ¦Ćļ”äņØś ĒÆŹņäĀņ£╝ļĪ£ ļŖśļĀż ļéśĻ░ĆļŖö ņŗØņ£╝ļĪ£ ņ¦äĒ¢ēĒĢ£ļŗż[5]. 4,166ļ¬ģņØś ĒÖśņ×ÉļōżņØ┤ ĒżĒĢ©ļÉ£ 52Ļ░£ņØś ņŚ░ĻĄ¼ļź╝ ļīĆņāüņ£╝ļĪ£ ĒĢ£ ļ®öĒāĆļČäņäØņŚÉ ņØśĒĢśļ®┤, 3~6Ļ░£ņøö ņČöņĀüņŚÉņä£ 83%ņØś ĒÖśņ×ÉņŚÉņä£ ņ”Øņāü ĒśĖņĀäņØä ļ│┤ņśĆļŗż[49]. ņ”ØņāüņØ┤ ņ׳ļŖö ņ£äņŗØļÅä ņŚŁļźśĻ░Ć 6Ļ░£ņøöņŚÉ 9% ņĀĢļÅä ļ░£ņāØĒĢ£ļŗżĻ│Ā ņĢīļĀżņĀĖ ņ׳Ļ│Ā, ņŗØļÅäņ▓£Ļ│ĄņØĆ 1.9% ņĀĢļÅäļĪ£ ņĢīļĀżņĀĖ ņ׳ņ£╝ļ®░, ņ▓£Ļ│ĄņØś Ēü¼ĻĖ░Ļ░Ć ņ×æņØä ļĢīļŖö ĻĖłņŗØ, ĒĢŁņāØņĀ£ Ēł¼ņŚ¼ ļśÉļŖö ņŖżĒģÉĒŖĖ ņéĮņ×ģ ņĀĢļÅäņØś ļ│┤ņĪ┤ņĀü ņ▓śņ╣śļĪ£ ņČ®ļČäĒĢśļéś, ņ▓£Ļ│ĄņØś Ēü¼ĻĖ░Ļ░Ć Ēü┤ Ļ▓ĮņÜ░ņŚÉļŖö ņłśņłĀņĀüņØĖ ņ▓śņ╣śĻ░Ć ņÜöĻĄ¼ļÉ£ļŗż[5,49]. ņŚ¼ļ¤¼ Ļ░ĆņØ┤ļō£ļØ╝ņØĖņŚÉ ļö░ļź┤ļ®┤ 1ĒśĢ ļśÉļŖö 2ĒśĢ ņŗØļÅä ņØ┤ņÖäļČłļŖźņØś Ļ▓ĮņÜ░ ĒÆŹņäĀ ĒÖĢņןņłĀņØä Ļ│ĀļĀżĒĢĀ ņłś ņ׳ņØä Ļ▓āņ£╝ļĪ£ ņāØĻ░üļÉ£ļŗż[5,19,21,49].
ļ│ĄĻ░ĢĻ▓Įņ£╝ļĪ£ ņŗØļÅä ņĀäļ▓Įņ£╝ļĪ£ ņĀæĻĘ╝ĒĢ┤ņä£ ņŗØļÅä ļÅīļ”╝ĻĘ╝ņ£ĪņĖĄĻ│╝ ņäĖļĪ£ĻĘ╝ņ£ĪņĖĄņØä ņ£äņŗØļÅä Ļ▓ĮĻ│äļČĆņŚÉņä£ ņāüļ░®ņ£╝ļĪ£ 5~7 cm, ĒĢśļ░®ņ£╝ļĪ£ 2 cm ņĀĢļÅäļź╝ ņĀłĻ░£ĒĢśļŖö Ļ▓āņ£╝ļĪ£, ļīĆņ▓┤ņĀüņ£╝ļĪ£ ņ£äņŗØļÅä ņŚŁļźśļź╝ ļ░®ņ¦ĆĒĢśĻĖ░ ņ£äĒĢ┤ņä£ ņ£äņĀĆļČĆ ņŻ╝ļ”äņłĀņØä Ļ░ÖņØ┤ ņŗ£Ē¢ēĒĢśļŖö Ļ▓ĮņÜ░Ļ░Ć ļ¦Äļŗż[5]. ļīĆļČĆļČäņØś ņŚ░ĻĄ¼ņŚÉņä£ 5ļģä ņČöņĀü Ļ▓Ćņé¼ņŚÉņä£ 90% ņØ┤ņāüņØś ņ”Øņāü ĒśĖņĀäņØä ļ│┤ņśĆļŗżĻ│Ā ļ│┤Ļ│ĀĒĢśĻ│Ā ņ׳ļŗż[5]. ņłśņłĀņØś ĒĢ®ļ│æņ”Øņ£╝ļĪ£ļŖö ņĀÉļ¦ē ņ▓£Ļ│Ą, ļ╣äņן ņåÉņāü, ĻĖ░ĒØē ļśÉļŖö ņČ£Ēśł ļō▒ņØ┤ ņĢīļĀżņĀĖ ņ׳ņ£╝ļéś ĻĘĖ ļ░£ņāØļźĀņØĆ ļ¦żņÜ░ ļé«ļŗżĻ│Ā ņĢīļĀżņĀĖ ņ׳ļŗż[50].
2010ļģäļīĆņŚÉ ļōżņ¢┤ņä£ Ē¢ēĒĢśņŚ¼ņ¦ĆĻ│Ā ņ׳ļŖö ņŗ£ņłĀņØ┤ļŗż. ņĀäņŗĀ ļ¦łņĘ©ĒĢśņŚÉņä£ ņżæļČĆ ļśÉļŖö ĒĢśļČĆņŗØļÅäņØś ņĀÉļ¦ē ņĀłĻ░£ļź╝ ņŗ£Ē¢ēĒĢśĻ│Ā ņØ┤ ņĀłĻ░£ļČĆļź╝ ĒåĄĒĢ┤ ļé┤ņŗ£Ļ▓Į ņäĀļŗ©ņØä ļäŻņ¢┤ ņĀÉļ¦ēĒĢśņĖĄņ£╝ļĪ£ ĒīīĻ│Āļōżņ¢┤Ļ░Ć ĒĢśļČĆņŗØļÅäņØś ļÅīļ”╝ĻĘ╝ņ£ĪņĖĄņØä ĒĢäņÜöĒĢ£ ļ¦īĒü╝ ņĀłĻ░£ĒĢ£ Ēøä ņĀÉļ¦ē ņĀłĻ░£ ļČĆņ£äļź╝ Ēü┤ļ”Į ļō▒ņ£╝ļĪ£ ļ┤ēĒĢ®ĒĢśļŖö ņŗ£ņłĀņØ┤ļŗż[49].
POEMņØä ĒĢśļŖö ļ░®ļ▓ĢņŚÉļŖö ņĀäļ░® Ēś╣ņØĆ Ēøäļ░® ņĀæĻĘ╝ņØś ļæÉ Ļ░Ćņ¦Ć ļ░®ļ▓ĢņØ┤ ņ׳ļŗż. ĒÖśņ×ÉĻ░Ć ņĢÖņÖĆņ£ä ņ×ÉņäĖļĪ£ ņ׳ļŖö ņāüĒā£ņŚÉņä£ ņĀäļ░® ĻĘ╝ņĀłĻ░£ļŖö 1ņŗ£ņŚÉņä£ 2ņŗ£ ļ░®Ē¢źņŚÉ ņŗ£ņłĀņØä ņŗ£Ē¢ēĒĢśĻ│Ā, Ēøäļ░® ĻĘ╝ņĀłĻ░£ļŖö 5ņŗ£ņŚÉņä£ 6ņŗ£ ļ░®Ē¢źņŚÉ ņŗ£ņłĀņØä ņŗ£Ē¢ēĒĢśĻ▓ī ļÉ£ļŗż[51]. ņØ┤ļĪĀņĀüņ£╝ļĪ£, ņĀäļ░® ĻĘ╝ņĀłĻ░£ļŖö ĒĢŁņŚŁļźś ĻĖ░ņĀäņ£╝ļĪ£ ņ×æņÜ®ĒĢśļŖö HisĻ░ü(angle of His), ņŖ¼ļ¦ü ĻĘ╝ņä¼ņ£Ā(sling muscle fiber)ņØś ņåÉņāü ņ£äĒŚśņØä ņżäņØ╝ ņłś ņ׳ņØä Ļ▓āņ£╝ļĪ£ ņāØĻ░üļÉ£ļŗż. Ēøäļ░® ĻĘ╝ņĀłĻ░£ļŖö ļīĆļČĆļČä ļé┤ņŗ£Ļ▓Į ņøīĒé╣ņ▒äļäÉņØ┤ 5ņŗ£ņŚÉņä£ 7ņŗ£ ņé¼ņØ┤ņŚÉ ņ£äņ╣śĒĢśĻĖ░ ļĢīļ¼ĖņŚÉ, ĻĘ╝ņĀłĻ░£ņŚÉ ņé¼ņÜ®ļÉśļŖö ļé┤ņŗ£Ļ▓Į ļÅäĻĄ¼ņÖĆņØś ņĀĢļĀ¼ļ®┤ņŚÉņä£ ņÜ░ņøöĒĢĀ ņłś ņ׳ņ£╝ļéś ĒĢŁņŚŁļźś ĻĖ░ņĀäņØä ļŗ┤ļŗ╣ĒĢśļŖö ņŖ¼ļ¦üĻĘ╝ņ£Ī(sling muscle)ņØś ņåÉņāüņØś ņ£äĒŚśņØ┤ ņ׳ņØä ņłś ņ׳ļŗż. ĒĢśņ¦Ćļ¦ī 1,247ļ¬ģņØś ĒÖśņ×Éļź╝ ļīĆņāüņ£╝ļĪ£ ĒĢ£ 18Ļ░£ ņŚ░ĻĄ¼ļź╝ ļČäņäØĒĢ£ ļ®öĒāĆļČäņäØņŚÉ ļö░ļź┤ļ®┤ ņĀäļ░® ĻĘ╝ņĀłĻ░£ņÖĆ Ēøäļ░® ĻĘ╝ņĀłĻ░£ ļ░®ļ▓Ģ ņé¼ņØ┤ņŚÉ ņ╣śļŻī ņä▒Ļ│ĄļźĀ, ņ£äņŗØļÅä ņŚŁļźś, ļČĆņ×æņÜ®ļ®┤ņŚÉņä£ ņ░©ņØ┤Ļ░Ć ņŚåņŚłļŗż[51]. Ēśäņ×¼ļĪ£ņä£ļŖö ņŗ£ņłĀņ×ÉņØś ņ×¼ļ¤ēņŚÉ ļö░ļØ╝ ĒĢ£ Ļ░Ćņ¦Ć ļ░®ļ▓ĢņØä ņäĀĒāØĒĢśĻ▓ī ļÉ£ļŗż. ļŗżļ¦ī ņØ┤ņĀä ņŗ£ņłĀļĪ£ ņØĖĒĢ£ ņåÉņāüņØ┤ ņŚåļŖö ļ░®Ē¢źņ£╝ļĪ£ ņĀæĻĘ╝ĒĢśļŖö Ļ▓āņØ┤ ĒĢ®ļ”¼ņĀüņ£╝ļĪ£ ļ│┤ņØĖļŗż. ņśłļź╝ ļōżņ¢┤ņä£ ņĀäļ▓Įņ£╝ļĪ£ ņĀæĻĘ╝ĒĢśļŖö ĒŚ¼ļ¤¼ ĻĘ╝ņĀłĻ░£ņłĀ Ēøä ņ╣śļŻīņŚÉ ņŗżĒī©ĒĢ£ Ļ▓ĮņÜ░ņŚÉļŖö ņØ┤ņĀä ņĀæĻĘ╝ĒĢ£ ļ░®Ē¢źĻ│╝ ļŗżļźĖ Ēøäļ░®ņ£╝ļĪ£ POEMņØä ĒĢśļŖö Ļ▓āņØ┤ ĒÜ©Ļ│╝ņĀüņØ╝ ņłś ņ׳ļŗż[52].
POEMņØĆ ļ│ĄĻ░ĢĻ▓Į ĒŚ¼ļ¤¼ ĻĘ╝ņĀłĻ░£ņłĀĻ│╝ ļŗ¼ļ”¼ ĒĢäņÜöĒĢ£ ļ¦īĒü╝ ĻĘ╝ņĀłĻ░£Ļ░Ć Ļ░ĆļŖźĒĢśļ»ĆļĪ£ ĒĢäņÜöĒĢśļŗżļ®┤ ņāüļČĆņŗØļÅäņŚÉņä£ļČĆĒä░ ņāüļČĆ ņ£äļČĆņ£äĻ╣īņ¦Ć ņĀłĻ░£Ļ░Ć Ļ░ĆļŖźĒĢśļŗżļŖö ņןņĀÉņØ┤ ņ׳ļŗż[49]. ļö░ļØ╝ņä£ 3ĒśĢ ņŗØļÅä ņØ┤ņÖäļČłļŖźņŚÉņä£ ļ¦żņÜ░ ļÅäņøĆņØ┤ ļÉśļŖö Ļ▓āņ£╝ļĪ£ ņĢīļĀżņĀĖ ņ׳ņ£╝ļ®░, ļ¼╝ļĪĀ 1, 2ĒśĢ ņŗØļÅä ņØ┤ņÖäļČłļŖźņŚÉņä£ļÅä ņŗ£Ē¢ēņØ┤ Ļ░ĆļŖźĒĢśļŗż[5,21,49]. ĒøäņłĀĒĢśĻ▓Āņ¦Ćļ¦ī, 1, 2, 3ĒśĢ ņŗØļÅä ņØ┤ņÖäļČłļŖź ļ¬©ļæÉņŚÉņä£ ĻĖ░ņĪ┤ņŚÉ ņō░ņØ┤ļŹś ĒÆŹņäĀ ĒÖĢņןņłĀļ│┤ļŗż ļéśņØĆ Ļ▓░Ļ│╝ļź╝ ļ│┤ņØ┤Ļ│Ā ņ׳ļŗż[53,54]. ĒĢśņ¦Ćļ¦ī POEM ņŗ£Ē¢ē ĒÖśņ×ÉņŚÉņä£ ĒŚ¼ļ¤¼ ĻĘ╝Ļ░£ņłĀĻ│╝ ļŗ¼ļ”¼ ņ£äņĀĆļČĆ ņŻ╝ļ”äņłĀ ļō▒ņØś ņ£äņŗØļÅä ņŚŁļźś ļ░®ņ¦Ć ņŗ£ņłĀņØä ļö░ļĪ£ ĒĢśņ¦Ć ņĢŖĻĖ░ ļĢīļ¼ĖņŚÉ ņāüļīĆņĀüņ£╝ļĪ£ ņ£äņŗØļÅä ņŚŁļźśĻ░Ć ņ×”ļŗżĻ│Ā ņĢīļĀżņĀĖ ņ׳ļŗż[5,29]. 2,373ļ¬ģņØś ĒÖśņ×ÉļōżņØä ļīĆņāüņ£╝ļĪ£ ĒĢ£ 36Ļ░£ņØś ņŚ░ĻĄ¼ļź╝ ļ░öĒāĢņ£╝ļĪ£ ĒĢ£ ļ®öĒāĆļČäņäØņŚÉ ņØśĒĢśļ®┤, 98%ņØś ņŗ£ņłĀņØ┤ Eckardt ņĀÉņłśĻ░Ć 3ņĀÉ ņØ┤ĒĢśļĪ£ ņä▒Ļ│ĄņĀüņØ┤ņŚłņ£╝ļéś ļ╣äņĀĢņāüņĀüņØĖ ņ£äņé░ ņŚŁļźśĻ░Ć 47%ņŚÉņä£ Ļ┤Ćņ░░ļÉśņŚłļŗżĻ│Ā ĒĢśņśĆļŗż[55]. ĒĢśņ¦Ćļ¦ī ņĄ£ĻĘ╝ ļśÉ ļŗżļźĖ ņŚ░ĻĄ¼ņŚÉ ņØśĒĢśļ®┤, POEM ņŗ£Ē¢ē ĒÖśņ×ÉļōżņŚÉņä£ ļ│┤Ē¢ēņä▒ ņé░ļÅä Ļ▓Ćņé¼ļź╝ ĒåĄĒĢśņŚ¼ ĒÖĢņØĖĒĢ£ ļ░öņŚÉ ņØśĒĢśļ®┤ ņāüļŗ╣ņłś ĒÖśņ×ÉļōżņŚÉņä£ ņŗØļÅäĻ│╝ļ»╝ņä▒ņŚÉ ņØśĒĢ£ ņ”ØņāüņØ╝ Ļ░ĆļŖźņä▒ļÅä ņĀ£ņŗ£ĒĢśĻ│Ā ņ׳ņ¢┤ ņČöĻ░ĆņĀüņØĖ ņŚ░ĻĄ¼Ļ░Ć ĒĢäņÜöĒĢĀ Ļ▓āņ£╝ļĪ£ ļ│┤ņØĖļŗż[56].
500ļ¬ģņØä ļīĆņāüņ£╝ļĪ£ ĒĢ£ Ēü░ ĻĘ£ļ¬©ņØś ļŗ©ņØ╝ĻĖ░Ļ┤Ć ņŚ░ĻĄ¼ņŚÉ ļö░ļź┤ļ®┤ POEMņØś ĒĢ®ļ│æņ”ØņØĆ 3.2%ļĪ£ ļ│┤Ļ│ĀļÉśņŚłņ£╝ļ®░, ļ¬©ļōĀ Ļ▓ĮņÜ░ņŚÉņä£ ļ│┤ņĪ┤ņĀü ņ╣śļŻīļĪ£ ņ╣śļŻīĻ░Ć Ļ░ĆļŖźĒĢśņśĆĻ│Ā ņé¼ļ¦ØĒĢ£ Ļ▓ĮņÜ░ļŖö ĒĢ£ Ļ▒┤ļÅä ņŚåņŚłļŗż[57]. ĒØöĒĢ£ ĒĢ®ļ│æņ”ØņØĆ Ļ│ĄĻĖ░ ņŻ╝ņ×ģĻ│╝ ņŚ░Ļ┤ĆļÉ£ ĒĢ®ļ│æņ”Ø, ņČ£Ēśł, ņĀÉļ¦ēņ▓£Ļ│ĄņØ┤ ņ׳Ļ│Ā, ņāüļīĆņĀüņ£╝ļĪ£ ĒØöĒĢśņ¦Ć ņĢŖņØĆ ĒĢ®ļ│æņ”Øņ£╝ļĪ£ļŖö ņóģĻ▓®ļÅÖņŚ╝, ļ│Ąļ¦ēņŚ╝, ĒØĪņØĖņä▒ ĒÅÉļĀ┤, ĒØēļ¦ē ņé╝ņČ£ņØ┤ ņ׳ļŗż[58]. ĻĖ░ļ│Ąņ”Ø, ņóģĻ▓®ļÅÖ ĻĖ░ņóģ, Ēö╝ĒĢśĻĖ░ņóģĻ│╝ Ļ░ÖņØ┤ Ļ│ĄĻĖ░ ņŻ╝ņ×ģĻ│╝ ņŚ░Ļ┤ĆļÉ£ ĒĢ®ļ│æņ”ØņØĆ Ļ░Ćņן ĒØöĒĢ£ ĒĢ®ļ│æņ”ØņØ┤ļ®░, 20%ņŚÉņä£ 30%ņØś ĒÖśņ×ÉņŚÉņä£ Ļ┤Ćņ░░ļÉśņ¦Ćļ¦ī ņ”ØņāüĻ│╝ ņŚ░Ļ┤Ćņä▒ņØä ļ│┤ņØ┤ņ¦Ć ņĢŖĻ│Ā ļ¼┤ņ”ØņāüņØĖ Ļ▓ĮņÜ░Ļ░Ć ļ¦Äļŗż[59]. ĒĢśņ¦Ćļ¦ī ĻĖ┤ņןņä▒ ĻĖ░ļ│Ąņ”ØĻ│╝ Ļ░ÖņØĆ ņŗ¼Ļ░üĒĢ£ ĒĢ®ļ│æņ”ØņØ┤ ļ░£ņāØĒĢ£ļŗżļ®┤ ļ│ĄĒåĄ ļ░Å ĒÖ£ļĀźņ¦ĢĒøäĻ░Ć ļČłņĢłņĀĢĒĢ┤ņ¦ł ņłś ņ׳Ļ│Ā, ņØ┤ļ¤░ Ļ▓ĮņÜ░ ļ░öļŖśĻ░ÉņĢĢņłĀņØ┤ ĒĢäņÜöĒĢĀ ņłśļÅä ņ׳ļŗż[60]. ņČ£ĒśłņØĆ 1.1%ņŚÉņä£ ļ░£ņāØĒĢśĻ│Ā, ņ¦ĆņŚ░ ņČ£ĒśłņØĆ 1% ļ»Ėļ¦īņŚÉņä£ ļ░£ņāØĒĢśļŖö Ļ▓āņ£╝ļĪ£ ļ│┤Ļ│ĀļÉśņ¢┤ ņ׳ļŗż[59]. ņĀÉļ¦ēņ▓£Ļ│ĄņØĆ ņŗ£ņłĀņ×ÉņØś ņłÖļĀ©ļÅäņŚÉ ļö░ļØ╝ 0%ņŚÉņä£ 25%Ļ╣īņ¦Ć ļŗżņ¢æĒĢśĻ▓ī ļ│┤Ļ│ĀļÉśĻ│Ā ņ׳ņ£╝ļéś ļ│┤ĒåĄ 10% ļ»Ėļ¦īņŚÉņä£ ļéśĒāĆļéśļ®░ ļīĆļČĆļČä ļé┤ņŗ£Ļ▓ĮņĀüņ£╝ļĪ£ ņ╣śļŻīĻ░Ć Ļ░ĆļŖźĒĢśļŗż[57,61]. ņŗØļÅäļłäņČ£ņØś Ļ▓ĮņÜ░ 0.3%ļĪ£ ļ│┤Ļ│ĀļÉśņ¢┤ ņ׳ļŗż[59].
POEMņØś ņ╣śļŻī ņä▒Ļ│ĄļźĀņØĆ ļ¦żņÜ░ ļåÆņ¦Ćļ¦ī, ņĀüņØĆ ņłśņŚÉņä£ļŖö ņŚ¼ņĀäĒ׳ ņ”ØņāüņØ┤ ņ¦ĆņåŹļÉśĻ▒░ļéś ņ×¼ļ░£ĒĢśļŖö Ļ▓ĮņÜ░Ļ░Ć ņāØĻĖ┤ļŗż. POEM ĒøäņŚÉ ņ”ØņāüņØ┤ ņ¦ĆņåŹļÉśĻ▒░ļéś ņ×¼ļ░£ĒĢ£ Ļ▓ĮņÜ░ ņ╣śļŻī ļ░®ļ▓ĢņŚÉ ļīĆĒĢ£ ļŹ░ņØ┤Ēä░ļŖö ļ¦Äņ¦Ć ņĢŖņ£╝ļéś, POEMņØä ļŗżņŗ£ ņŗ£Ē¢ēĒĢśĻ▒░ļéś ĒŚ¼ļ¤¼ ĻĘ╝ņĀłĻ░£ņłĀņØä Ļ│ĀļĀżĒĢ┤ ļ│╝ ņłś ņ׳ļŗż. ĒĢ£ ļŗ©ņØ╝ĻĖ░Ļ┤Ć ņŚ░ĻĄ¼ņŚÉ ļö░ļź┤ļ®┤ 441ļ¬ģņØś ĒÖśņ×ÉņŚÉ ļīĆĒĢ┤ POEMņØä ņŗ£Ē¢ēĒĢśņśĆņØä ļĢī, 3ļģä ļé┤ņŚÉ 43ļ¬ģ(9.8%)ņØś ĒÖśņ×ÉņŚÉņä£ ņ”ØņāüņØ┤ ņ¦ĆņåŹļÉśĻ▒░ļéś ņ×¼ļ░£ĒĢśņśĆļŗż. ņ”ØņāüņØ┤ ņ¦ĆņåŹļÉśĻ▒░ļéś ņ×¼ļ░£ĒĢ£ ĒÖśņ×É ņżæ 34ļ¬ģ(8%)ņØś ĒÖśņ×ÉļōżņØĆ ņ×¼ņ╣śļŻīļź╝ ļ░øņĢśļŖöļŹ░, ņ×¼ņ╣śļŻīļĪ£ ļ│ĄĻ░ĢĻ▓Į ĒŚ¼ļ¤¼ ĻĘ╝ņĀłĻ░£ņłĀņØĆ 45%, POEMņØĆ 63%ņŚÉņä£ ĒÜ©Ļ│╝Ļ░Ć ņ׳ņŚłļŗż. ļ░śļ®┤ņŚÉ ĒÆŹņäĀ ĒÖĢņןņłĀņØĆ 0%ņŚÉņä£ 20%ļĪ£ ņāüļīĆņĀüņ£╝ļĪ£ ĒÜ©Ļ│╝Ļ░Ć ņóŗņ¦Ć ņĢŖņĢśļŗż[62]. ĒĢ£ ļŗżĻĖ░Ļ┤Ć ņŚ░ĻĄ¼ņŚÉ ļö░ļź┤ļ®┤ 46ļ¬ģņØś ĒÖśņ×ÉņŚÉ ļīĆĒĢ┤ POEM Ēøä ņ”ØņāüņØ┤ ņ׳ņ¢┤ņä£ ļŗżņŗ£ POEMņØä ņŗ£Ē¢ēĒĢśņśĆņØä ļĢī, ļ¬©ļōĀ ĒÖśņ×ÉņŚÉņä£ ĻĖ░ņłĀņĀüņ£╝ļĪ£ ņä▒Ļ│ĄĒĢśņśĆĻ│Ā, 41ļ¬ģ(85%)ņŚÉņä£ Eckardt ņĀÉņłśĻ░Ć 3ņĀÉ ņØ┤ĒĢśļĪ£ ņ”Øņāü ĒśĖņĀäņØä ļ│┤ņśĆļŗż. POEM Ēøä ņ”ØņāüņØ┤ ņ¦ĆņåŹļÉśĻ▒░ļéś ņ×¼ļ░£ĒĢ£ Ļ▓ĮņÜ░ ņ×¼ņ╣śļŻī ļ░®ļ▓Ģņ£╝ļĪ£ POEMĻ│╝ ĒŚ¼ļ¤¼ ĻĘ╝ņĀłĻ░£ņłĀ ņżæ ņ¢┤ļ¢ż ļ░®ļ▓ĢņØ┤ ļŹö ņÜ░ņøöĒĢ£ņ¦ĆņŚÉ ļīĆĒĢ┤ņä£ļŖö ņČöĒøä ļ¼┤ņ×æņ£ä ļīĆņĪ░ĻĄ░ ņŚ░ĻĄ¼ ļō▒ņØś ņČöĻ░Ć ņŚ░ĻĄ¼Ļ░Ć ĒĢäņÜöĒĢśļŗż[63].
ņĢäņ¦üĻ╣īņ¦Ć ņןĻĖ░Ļ░ä ļ╣äĻĄÉ ņŚ░ĻĄ¼ļŖö ņŚåņ£╝ļéś POEMĻ│╝ ļ│ĄĻ░ĢĻ▓Į ĒŚ¼ļ¤¼ ĻĘ╝ņĀłĻ░£ņłĀ ļ¼┤ņ×æņ£ä ļ╣äĻĄÉņŚÉņä£ ļ╣äņŚ┤ļō▒ĒĢ©ņØ┤ ņ”Øļ¬ģļÉśņŚłĻ│Ā ņ”Øņāü ĒśĖņĀäņØ┤ 2ļģäĻ╣īņ¦Ć ņ£Āņ¦ĆļÉśņŚłļŗż[64]. ĒĢśņ¦Ćļ¦ī ņ£äņŗØļÅä ņŚŁļźśĻ░Ć POEMĻĄ░ņŚÉņä£ ņĪ░ĻĖł ļŹö ļ¦ÄņØ┤ Ļ┤Ćņ░░ļÉśņŚłļŗż(POEMĻĄ░ņŚÉņä£ 44% vs. ĒŚ¼ļ¤¼ ĻĘ╝ņĀłĻ░£ņłĀ ļ░Å ņ£äņĀĆļČĆ ņŻ╝ļ”äņłĀĻĄ░ņŚÉņä£ 29%) [64]. ļśÉ ļŗżļźĖ POEMĻ│╝ ĒÆŹņäĀ ĒÖĢņןņłĀ ļ¼┤ņ×æņ£ä ļ╣äĻĄÉ ņŚ░ĻĄ¼ņŚÉņä£ļŖö ĒÆŹņäĀ ĒÖĢņןņłĀņŚÉ ļ╣äĒĢ┤ POEMņØ┤ 2ļģä Ļ┤Ćņ░░ņŚÉņä£ Ēø©ņö¼ ņóŗņØĆ Ļ▓░Ļ│╝ļź╝ ļ│┤ņśĆļŗż(95% vs. 54%) [54]. POEMņØĆ ĒŖ╣Ē׳ 3ĒśĢ ņŗØļÅä ņØ┤ņÖäļČłļŖźņ”ØņŚÉņä£ ĒÜ©Ļ│╝ņĀüņØ┤ņŚłļŗż[54].
ĒĢ®ļ│æņ”Øņ£╝ļĪ£ ĒØĪņØĖņä▒ ĒÅÉļĀ┤ņØ┤ļéś ĒśĖĒØĪĻĖ░ Ļ░ÉņŚ╝ ĻĘĖļ”¼Ļ│Ā ĒÄĖĒÅēņäĖĒżņŗØļÅäņĢö ļō▒ņØ┤ ņØ╝ļ░śņØĖņŚÉ ņāüļīĆņĀüņ£╝ļĪ£ ļåÆņØĆ Ļ▓āņ£╝ļĪ£ ņĢīļĀżņĀĖ ņ׳Ļ│Ā, ļīĆļČĆļČäņØś ņŗØļÅäņĢöņØĆ ņŗØļÅä ņØ┤ņÖäļČłļŖź 10ļģä ņØ┤ĒøäņŚÉ Ļ┤Ćņ░░ļÉ£ļŗżĻ│Ā ņĢīļĀżņĀĖ ņ׳ļŗż[65].
ņŗØļÅä ņØ┤ņÖäļČłļŖźņØĆ ņĄ£ĻĘ╝ ņāłļĪ£ņÜ┤ ļé┤ņŗ£Ļ▓Į ņŗ£ņłĀ ļ░Å ņāłļĪ£ņÜ┤ ņ¦äļŗ©ļ▓ĢņØä ĒåĄĒĢśņŚ¼ ņ¦äļŗ© ļ░Å ņ╣śļŻīĻ░Ć Ļ│äņåŹĒĢ┤ņä£ ļ░£ņĀäĒĢśĻ│Ā ņ׳ļŖö ņżæņØ┤ļŗż. ņØ┤ļ¤¼ĒĢ£ ņāłļĪ£ņÜ┤ ņ¦äļŗ© ļ░Å ņ╣śļŻīņŚÉ ļīĆĒĢ£ ņČ®ļČäĒĢ£ ņØ┤ĒĢ┤ļź╝ ĒåĄĒĢśņŚ¼ ņé╝Ēé┤Ļ│żļ×ĆņØä ņŻ╝ņåīļĪ£ ļé┤ņøÉĒĢśļŖö ĒÖśņ×Éļōż ņ¦äļŗ©ĒĢ£ļŗżļ®┤ Ļ▒░ĻĖ░ņŚÉ ļ¦×ļŖö ņś¼ļ░öļźĖ ņ╣śļŻīļź╝ ĒĢĀ ņłś ņ׳ņØä Ļ▓āņ£╝ļĪ£ ņāØĻ░üļÉ£ļŗż[32].
Acknowledgements
This study was financially supported by a grant of the Korean Society of Neurogastroenterology and Motility (KSNM-20-02).
Fig.┬Ā1.
High-resolution manometry set-up. The equipment comprises a 12-French catheter with 36 pressure sensors at 1-cm intervals and 18 impedance sensors at 2-cm intervals (Diversatek Healthcare, Milwaukee, WI, USA). When the catheter is positioned into the esophagus, the sensors detect the pressure in various parts of the esophagus. Intraluminal pressure data are converted into dynamic esophageal pressure topography plots by integrated software algorithms.
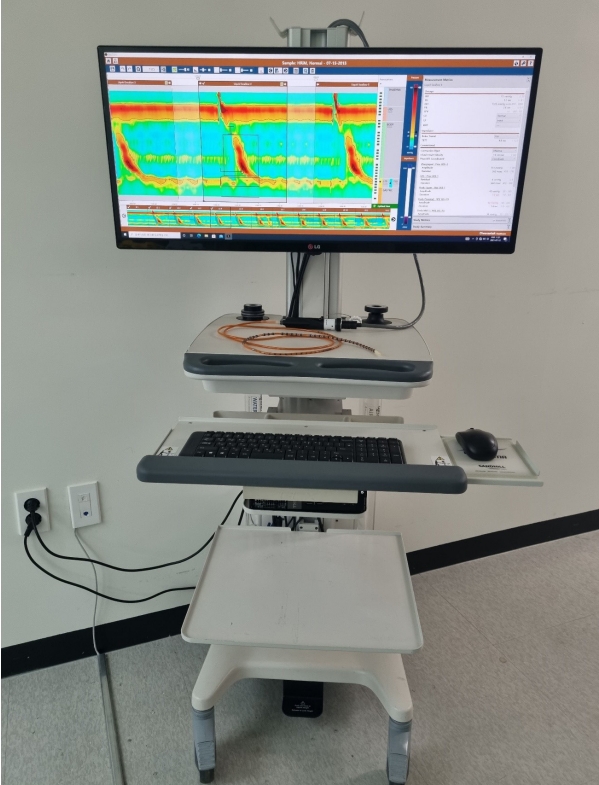
Fig.┬Ā2.
Representative high-resolution manometric images of normalcy and achalasia. (A) Normal finding: the black box represents 10 seconds of the post-swallow period. Integrated relaxation pressure (IRP) is defined as the median 4 seconds nadir of pressure through the esophagogastric junction in the black box. IRP is decreased during the post-swallow period. (B) Achalasia type I: the IRP is elevated, and failed peristalsis is noted. (C) Achalasia type II: the IRP is elevated, and panesophageal pressurization is noted. (D) Achalasia type III: the IRP is elevated, and spasm is noted.

Table┬Ā1.
Main Differences between Versions 3.0 and 4.0 of the Chicago Classification
REFERENCES
2. Khan A, Yadlapati R, Gonlachanvit S, et al. Chicago classification update (version 4.0): technical review on diagnostic criteria for achalasia. Neurogastroenterol Motil 2021;33:e14182.



4. Yadlapati R, Kahrilas PJ, Fox MR, et al. Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0┬®. Neurogastroenterol Motil 2021;33:e14058.


6. van Hoeij FB, Ponds FA, Smout AJ, Bredenoord AJ. Incidence and costs of achalasia in the Netherlands. Neurogastroenterol Motil 2018;30:e13195.


7. Sadowski DC, Ackah F, Jiang B, Svenson LW. Achalasia: incidence, prevalence and survival. A population-based study. Neurogastroenterol Motil 2010;22:e256ŌĆōe261.


8. Samo S, Carlson DA, Gregory DL, Gawel SH, Pandolfino JE, Kahrilas PJ. Incidence and prevalence of achalasia in central Chicago, 2004-2014, since the widespread use of high-resolution manometry. Clin Gastroenterol Hepatol 2017;15:366ŌĆō373.



9. Duffield JA, Hamer PW, Heddle R, Holloway RH, Myers JC, Thompson SK. Incidence of achalasia in South Australia based on esophageal manometry findings. Clin Gastroenterol Hepatol 2017;15:360ŌĆō365.


10. Kim E, Lee H, Jung HK, Lee KJ. Achalasia in Korea: an epidemiologic study using a national healthcare database. J Korean Med Sci 2014;29:576ŌĆō580.




11. Jung KW, Jung HY, Yoon IJ, et al. Basal and residual lower esophageal pressures increase in old age in classic achalasia, but not vigorous achalasia. J Gastroenterol Hepatol 2010;25:1452ŌĆō1455.


12. Becker J, Haas SL, Mokrowiecka A, et al. The HLA-DQ╬▓1 insertion is a strong achalasia risk factor and displays a geospatial north-south gradient among Europeans. Eur J Hum Genet 2016;24:1228ŌĆō1231.




13. Jung KW, Yoon IJ, Kim DH, et al. Genetic evaluation of ALADIN gene in early-onset achalasia and alacrima patients. J Neurogastroenterol Motil 2011;17:169ŌĆō173.



14. Spechler SJ, Konda V, Souza R. Can eosinophilic esophagitis cause achalasia and other esophageal motility disorders? Am J Gastroenterol 2018;113:1594ŌĆō1599.



15. Nelson M, Zhang X, Genta RM, et al. Lower esophageal sphincter muscle of patients with achalasia exhibits profound mast cell degranulation. Neurogastroenterol Motil 2021;33:e14055.



16. Booy JD, Takata J, Tomlinson G, Urbach DR. The prevalence of autoimmune disease in patients with esophageal achalasia. Dis Esophagus 2012;25:209ŌĆō213.


17. King D, Thomas T, Chandan JS, et al. Achalasia is associated with atopy in patients younger than 40 years of age. Am J Gastroenterol 2021;116:416ŌĆō419.


18. Jung DH, Park H. Is gastroesophageal reflux disease and achalasia coincident or not? J Neurogastroenterol Motil 2017;23:5ŌĆō8.



19. Jung HK, Hong SJ, Lee OY, et al. 2019 Seoul consensus on esophageal achalasia guidelines. J Neurogastroenterol Motil 2020;26:180ŌĆō203.



20. Patel DA, Sharda R, Hovis KL, et al. Patient-reported outcome measures in dysphagia: a systematic review of instrument development and validation. Dis Esophagus 2017;30:1ŌĆō23.



21. Vaezi MF, Pandolfino JE, Yadlapati RH, Greer KB, Kavitt RT. ACG clinical guidelines: diagnosis and management of achalasia. Am J Gastroenterol 2020;115:1393ŌĆō1411.



22. Gyawali CP, Kahrilas PJ. A short history of high-resolution esophageal manometry. Dysphagia, 2021. doi: 10.1007/s00455-021-10372-7. [Epub ahead of print].
23. Fox MR, Bredenoord AJ. Oesophageal high-resolution manometry: moving from research into clinical practice. Gut 2008;57:405ŌĆō423.


24. Linehan JH, Dent J, Dodds WJ, Hogan WJ. Sleeve device functions as a starling resistor to record sphincter pressure. Am J Physiol 1985;248(2 Pt 1): G251ŌĆōG255.


25. Clouse RE, Staiano A, Alrakawi A, Haroian L. Application of topographical methods to clinical esophageal manometry. Am J Gastroenterol 2000;95:2720ŌĆō2730.


26. Clouse RE. Topographic manometry: an evolving method for motility. J Pediatr Gastroenterol Nutr 2001;32 Suppl 1:S10ŌĆōS11.


27. Ghosh SK, Pandolfino JE, Rice J, Clarke JO, Kwiatek M, Kahrilas PJ. Impaired deglutitive EGJ relaxation in clinical esophageal manometry: a quantitative analysis of 400 patients and 75 controls. Am J Physiol Gastrointest Liver Physiol 2007;293:G878ŌĆōG885.


28. Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, Kahrilas PJ. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology 2008;135:1526ŌĆō1533.



29. Patel DA, Yadlapati R, Vaezi MF. Esophageal motility disorders: current approach to diagnostics and therapeutics. Gastroenterology 2022;162:1617ŌĆō1634.


30. Lin Z, Kahrilas PJ, Roman S, Boris L, Carlson D, Pandolfino JE. Refining the criterion for an abnormal integrated relaxation pressure in esophageal pressure topography based on the pattern of esophageal contractility using a classification and regression tree model. Neurogastroenterol Motil 2012;24:e356ŌĆōe363.



31. Carlson DA, Roman S. Esophageal provocation tests: are they useful to improve diagnostic yield of high resolution manometry? Neurogastroenterol Motil 2018;30:e13321.



32. Jung KW. Chicago classification ver. 4.0: diagnosis of achalasia and esophagogastric junction outflow obstruction. Korean J Gastroenterol 2022;79:61ŌĆō65.


33. Hsing LC, Jung KW. Role of the rapid drink challenge test in esophageal motility disorder diagnosis. J Neurogastroenterol Motil 2020;26:167ŌĆō168.



34. Dall FH, J├Ėrgensen CS, Houe D, Gregersen H, Djurhuus JC. Biomechanical wall properties of the human rectum. A study with impedance planimetry. Gut 1993;34:1581ŌĆō1586.



35. Gregersen H, Djurhuus JC. Impedance planimetry: a new approach to biomechanical intestinal wall properties. Dig Dis 1991;9:332ŌĆō340.



36. Pandolfino JE, Shi G, Zhang Q, Ghosh S, Brasseur JG, Kahrilas PJ. Measuring EGJ opening patterns using high resolution intraluminal impedance. Neurogastroenterol Motil 2005;17:200ŌĆō206.


37. Lin Z, Nicod├©me F, Boris L, Lin CY, Kahrilas PJ, Pandolfino JE. Regional variation in distal esophagus distensibility assessed using the functional luminal imaging probe (FLIP). Neurogastroenterol Motil 2013;25:e765ŌĆōe771.



38. Kwiatek MA, Kahrilas K, Soper NJ, et al. Esophagogastric junction distensibility after fundoplication assessed with a novel functional luminal imaging probe. J Gastrointest Surg 2010;14:268ŌĆō276.




39. Kwiatek MA, Pandolfino JE, Hirano I, Kahrilas PJ. Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP). Gastrointest Endosc 2010;72:272ŌĆō278.



40. Cha B, Jung KW. Diagnosis of dysphagia: high resolution manometry & EndoFLIP. Korean J Gastroenterol 2021;77:64ŌĆō70.


41. Savarino E, di Pietro M, Bredenoord AJ, et al. Use of the functional lumen imaging probe in clinical esophagology. Am J Gastroenterol 2020;115:1786ŌĆō1796.



42. Carlson DA, Gyawali CP, Kahrilas PJ, et al. Esophageal motility classification can be established at the time of endoscopy: a study evaluating real-time functional luminal imaging probe panometry. Gastrointest Endosc 2019;90:915ŌĆō923.e1.



43. Carlson DA, Gyawali CP, Khan A, et al. Classifying esophageal motility by FLIP panometry: a study of 722 subjects with manometry. Am J Gastroenterol 2021;116:2357ŌĆō2366.



44. Blonski W, Kumar A, Feldman J, Richter JE. Timed barium swallow: diagnostic role and predictive value in untreated achalasia, esophagogastric junction outflow obstruction, and non-achalasia dysphagia. Am J Gastroenterol 2018;113:196ŌĆō203.


45. Ratuapli SK, Crowell MD, DiBaise JK, et al. Opioid-induced esophageal dysfunction (OIED) in patients on chronic opioids. Am J Gastroenterol 2015;110:979ŌĆō984.



46. Kim GH, Jung KW. The role of opioids and alcohol in the development of achalasia type III and esophagogastric junction outflow obstruction. J Neurogastroenterol Motil 2019;25:177ŌĆō178.



47. Kim GH, Jung KW. Emerging issues in esophageal motility diseases. Korean J Gastroenterol 2019;73:322ŌĆō326.



48. Campos GM, Vittinghoff E, Rabl C, et al. Endoscopic and surgical treatments for achalasia: a systematic review and metaanalysis. Ann Surg 2009;249:45ŌĆō57.

49. Khashab MA, Vela MF, Thosani N, et al. ASGE guideline on the management of achalasia. Gastrointest Endosc 2020;91:213ŌĆō227.e6; .


50. Zaninotto G, Bennett C, Boeckxstaens G, et al. The 2018 ISDE achalasia guidelines. Dis Esophagus 2018;31:1ŌĆō29.
51. Mohan BP, Ofosu A, Chandan S, et al. Anterior versus posterior approach in peroral endoscopic myotomy (POEM): a systematic review and meta-analysis. Endoscopy 2020;52:251ŌĆō258.


52. Li QL, Zhou PH. Perspective on peroral endoscopic myotomy for achalasia: Zhongshan experience. Gut Liver 2015;9:152ŌĆō158.



53. Kim GH, Jung KW, Jung HY, et al. Superior clinical outcomes of peroral endoscopic myotomy compared with balloon dilation in all achalasia subtypes. J Gastroenterol Hepatol 2019;34:659ŌĆō665.



54. Ponds FA, Fockens P, Lei A, et al. Effect of peroral endoscopic myotomy vs pneumatic dilation on symptom severity and treatment outcomes among treatment-naive patients with achalasia: a randomized clinical trial. JAMA 2019;322:134ŌĆō144.



55. Akintoye E, Kumar N, Obaitan I, Alayo QA, Thompson CC. Peroral endoscopic myotomy: a meta-analysis. Endoscopy 2016;48:1059ŌĆō1068.


56. Ponds FA, Oors JM, Smout AJPM, Bredenoord AJ. Reflux symptoms and oesophageal acidification in treated achalasia patients are often not reflux related. Gut 2021;70:30ŌĆō39.



57. Inoue H, Sato H, Ikeda H, et al. Per-oral endoscopic myotomy: a series of 500 patients. J Am Coll Surg 2015;221:256ŌĆō264.


58. Pannala R, Abu Dayyeh BK, Aslanian HR, et al. Per-oral endoscopic myotomy (with video). Gastrointest Endosc 2016;83:1051ŌĆō1060.


59. Patel K, Abbassi-Ghadi N, Markar S, Kumar S, Jethwa P, Zaninotto G. Peroral endoscopic myotomy for the treatment of esophageal achalasia: systematic review and pooled analysis. Dis Esophagus 2016;29:807ŌĆō819.


60. McGrath B, Calderon LF, Xie M, et al. Delayed tension symptomatic pneumoperitoneum after POEM requiring needle decompression. Am J Gastroenterol 2021;116:407ŌĆō410.


61. Bechara R, Ikeda H, Inoue H. Peroral endoscopic myotomy: an evolving treatment for achalasia. Nat Rev Gastroenterol Hepatol 2015;12:410ŌĆō426.



62. van Hoeij FB, Ponds FA, Werner Y, et al. Management of recurrent symptoms after per-oral endoscopic myotomy in achalasia. Gastrointest Endosc 2018;87:95ŌĆō101.


63. Tyberg A, Seewald S, Sharaiha RZ, et al. A multicenter international registry of redo per-oral endoscopic myotomy (POEM) after failed POEM. Gastrointest Endosc 2017;85:1208ŌĆō1211.


64. Werner YB, Hakanson B, Martinek J, et al. Endoscopic or surgical myotomy in patients with idiopathic achalasia. N Engl J Med 2019;381:2219ŌĆō2229.


-
METRICS

-
- 1 Crossref
- 2,549 View
- 79 Download
- Related articles in Korean J Helicobacter Up Gastrointest Res