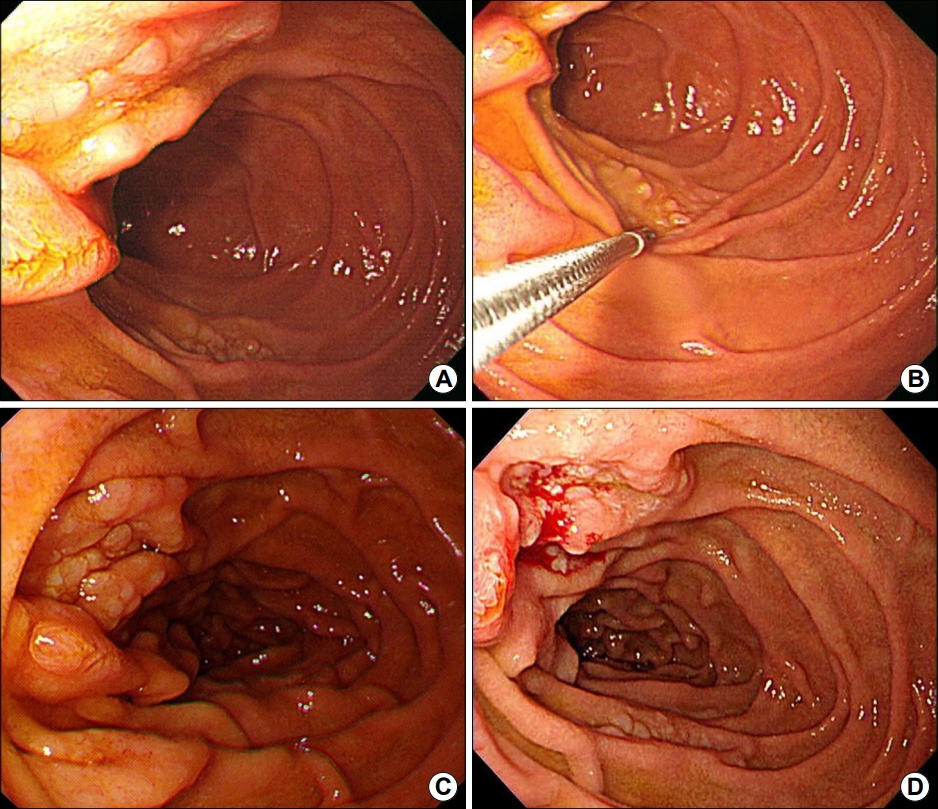
Question: A 40-year old man presented with duodenal mucosal nodularity incidentally found in a screening esophagogastroduodenoscopy (EGD). He did not have any abnormal symptoms nor recent weight loss. He was taking medicine for hypertension and dyslipidemia since 1 year ago and was non-smoker and social drinker. His laboratory findings were all within normal limit. On EGD, nonspecific slightly pale grayish mucosal nodularity was found on the second portion of duodenum, around the ampulla of Vater and in about 1~2 cm distal area from the ampulla (Fig. 1A, B). Colonoscopy and abdomino-pelvic CT scan revealed no abnormal findings.
What is the most likely diagnosis?
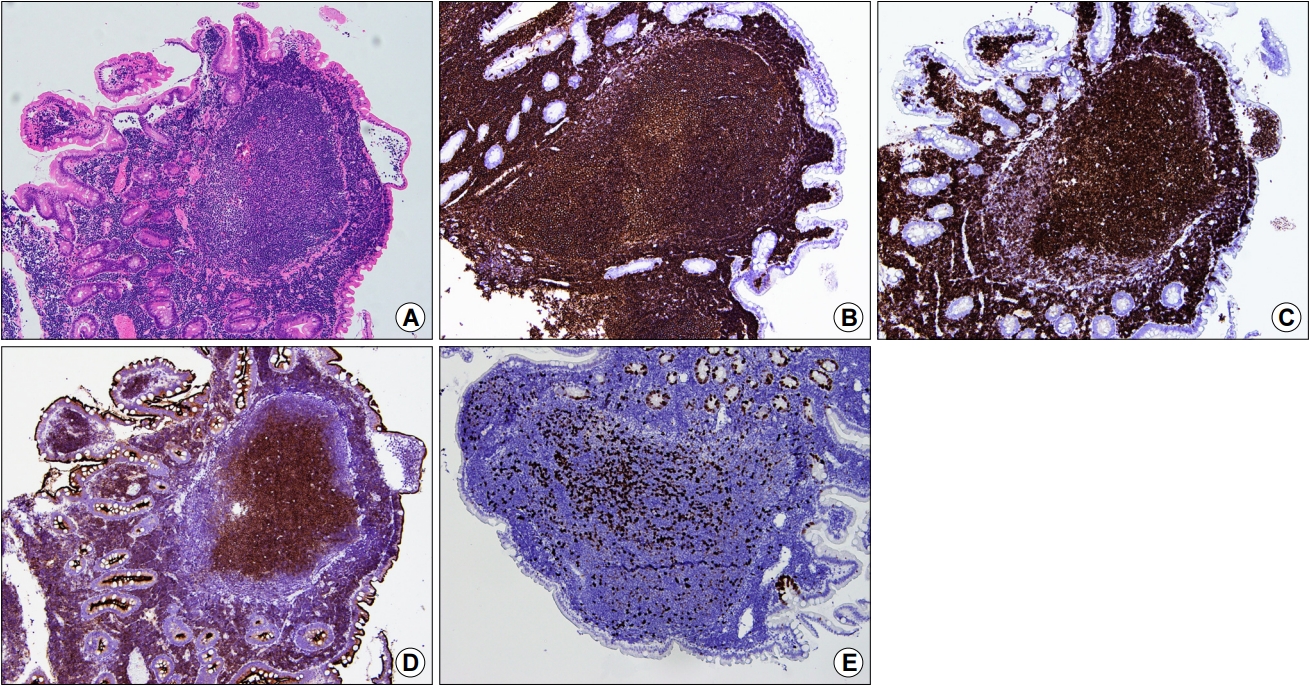
Answer: Urea breath test showed negative result. In the follow-up EGD, diffuse mucosal nodularity around the ampulla of Vater was shown in the second portion of duodenum (Fig. 1C). Biopsy revealed dense infiltration of lymphoid cells in the lamina propria, forming follicles (Fig. 2). As this finding was highly suggestive of malignant lymphoma, immunohistochemistry was performed and showed CD20, CD10, and B-cell lymphoma 2 (BCL-2) positive, CD3/CD5 negative, and Ki-67 positive in 5%.
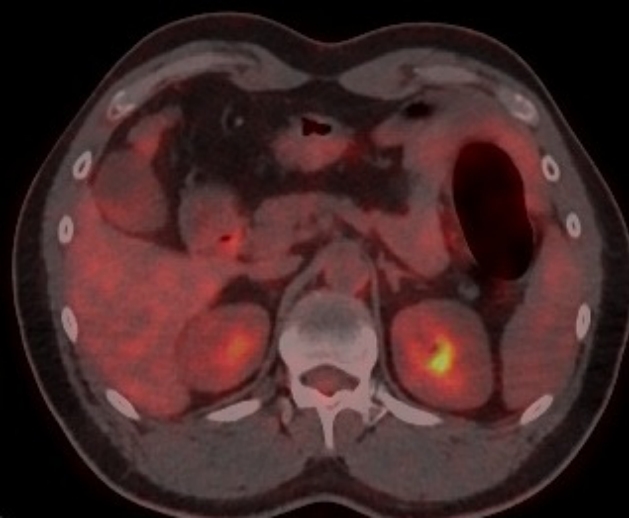
This finding was consistent with grade 1 to 2 follicular lymphoma. Therefore, whole body positron emission tomography scan was performed for staging, and it revealed mild hypermetabolic lesion in duodenum (Fig. 3). Bone marrow examination was performed and it was normal. His modified Ann Arbor stage was determined as IE1. After discussion with oncology professional, he was decided to be observed without treatment. Six months later, follow-up EGD revealed no interval change and biopsy was performed at the periampullary nodularity (Fig. 1D), which revealed the same result as previous one. He is under follow-up without any symptoms.
Primary gastrointestinal follicular lymphoma is a rather rare disease, although the gastrointestinal tract is the most common site of extranodal lymphoma [1]. Although rare, when follicular lymphoma involves the gastrointestinal tract, the duodenum is the most commonly affected site. Most of the cases of duodenal follicular lymphoma are asymptomatic and its specific risk factors are unknown [2]. Unlike non-gastrointestinal follicular lymphoma, primary gastrointestinal follicular lymphoma shows remarkably indolent behavior. It shares some features with mucosa-associated lymphoid tissue (MALT) lymphoma. However unlike MALT lymphoma, duodenal follicular lymphoma does not show marginal zone differentiation. Also MALT lymphoma is often negative for CD10 because of its origin from post-germinal center memory B cells [3].
Old studies have suggested local radiation therapy for limited stage follicular lymphoma, however Stanford University first advocated watch-and-wait strategy according to the result of their two retrospective studies [4,5]. A retrospective study including 63 cases of duodenal follicular lymphoma reported good prognosis after heterogeneous treatments including watch-and-wait, radiation, Rituximab, and chemotherapy [6]. Among them seven patients reached complete remission without treatment. In 2016, World Health Organization recognized this entity as one distinct form of duodenal type follicular lymphoma [7]. However, there is still no established consensus on the initial treatment modality [8]. Most oncologists either take a ŌĆ£watch-and-waitŌĆØ strategy, or some treat with local radiation. More recently, some tried rituximab or even chemotherapy. However, for asymptomatic, low grade, limited stage duodenal follicular lymphoma, chemotherapy is generally not recommended and watch-and-wait can be a good option [3].