A Case of Gastric Mixed Neuroendocrine-Nonneuroendocrine Neoplasm Composed With Adenoma and Neuroendocrine Tumor
Article information
Abstract
Mixed neuroendocrine-nonneuroendocrine neoplasms (MiNENs) of the gastrointestinal tract, particularly gastric MiNENs are rare, and a gastric adenoma that occurs concomitant with a neuroendocrine carcinoma (and not gastric adenocarcinoma) is extremely rare. The clinicopathologic and pathogenetic features of MiNENs remain unclear, and treatment guidelines are currently unavailable. A 75-year-old man patient was referred to our hospital for management of a gastric adenoma. Endoscopy revealed an elevated mucosal lesion (10 mm×10 mm) at the greater curvature of the lower gastric body. The patient underwent endoscopic submucosal dissection for removal of the gastric neoplasm. Histopathological evaluation revealed mixed epithelial dysplasia, low and partly high grade and a neuroendocrine tumor (grade 1). Immunohistochemical analysis showed neoplastic cells with immunopositivity for CD56, synaptophysin, and INSM1, and Ki-67 showed 2.2%. Therefore, the patient was diagnosed with a low-grade gastric MiNEN. We present a rare case of gastric MiNENs (adenoma-neuroendocrine tumor) together with a literature review.
INTRODUCTION
Mixed neuroendocrine-nonneuroendocrine neoplasms (Mi-NENs) can occur in any organ of the digestive system, with the highest frequency in the colon. MiNENs are mixtures that contain both neuroendocrine (NE) and non-NE components, and each component occupies at least 30% of the total tumor volume individually. The World Health Organization (WHO) 2010 classification recommended the term mixed adeno-neuroendocrine carcinoma (MANEC) for these tumors, but due to its limitations in not adequately addressing the heterogeneity of possible combinations of NE (well-differentiated or poorly-differentiated) and non-NE (e.g., adenocarcinoma, squamous cell carcinoma, or adenoma) phenotypes, the 2019 WHO classification changed the term to MiNENs [1,2]. These neoplasms were stratified into various prognostic categories based on the malignancy of each component, with mixed adenomas and welldifferentiated neuroendocrine tumors (MANETs) being classified as low-grade MiNENs.
MiNENs of the stomach, are rare, moreover, lesions with a combination of endocrine tumors and gastric adenomas which are specific low-grade MiNENs, have been reported even more rarely. Therefore, our understanding of their pathogenesis, clinical presentation and prognosis, and optimal treatment approaches is currently limited.
We would like to report a case of MiNEN with gastric adenoma and neuroendocrine tumor (NET) in a patient who underwent endoscopic submucosal dissection (ESD) for suspected gastric adenoma detected on a screening endoscopy.
CASE REPORT
A 75-year-old man patient was referred from a local clinic due to a suspected gastric adenoma detected on a screening upper endoscopy. The patient’s medical history was unremarkable except for a history of hypertension. There were no specific findings in the blood test performed at the time of admission.
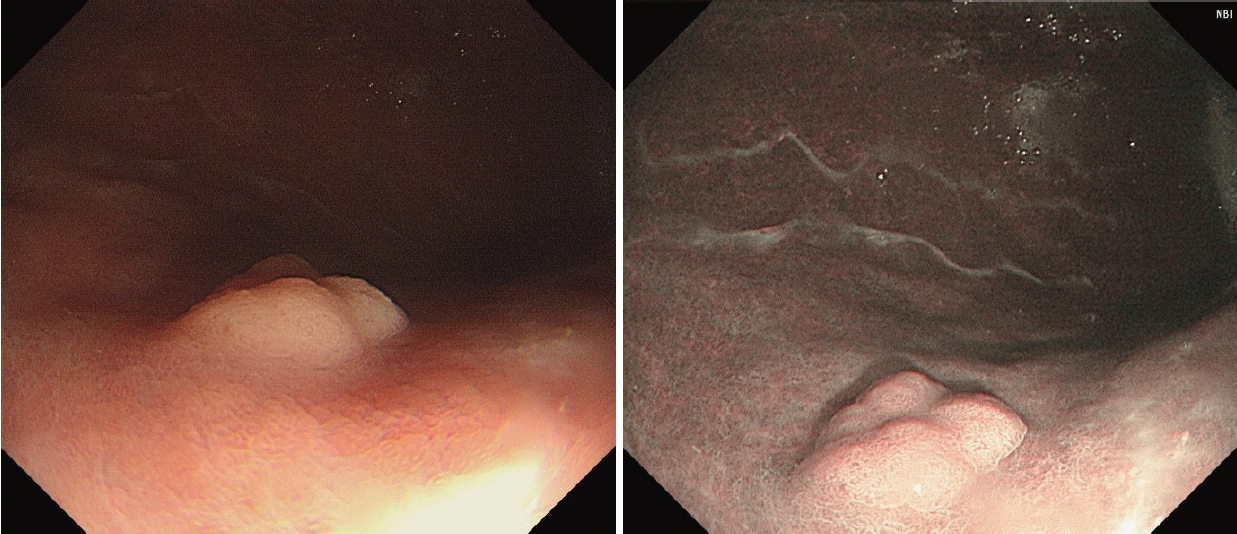
On upper gastrointestinal endoscopy, there was about 10 mm sized, ovoid, superficial-elevated mucosal lesion noted at the greater curvature of the lower body (Fig. 1). Histopathological examination of the endoscopic biopsy specimen showed tubular adenoma, and low-grade dysplasia.
Based on pathological findings, the patient underwent ESD for a gastric lesion is suspected of adenoma (Fig. 2). The exact tumor size was 10×8 mm. The depth of invasion was confined to the muscularis mucosa, and there was no lymphovascular invasion or extension of the resection margin. Microscopic examination of the completely resected specimen with hematoxylin and eosin staining showed slightly elevated lesions with many superficial tubular or dilated glands without fusing (Fig. 3A). The NE-type cells are observed in the deep mucosa and submucosa along with adenomatous cells in the superficial part of the mucosa, which are more clearly seen on immunochemistry. Many cords and sheets of small NE-type cells that formed small clusters or sheets were observed (Fig. 3B). Immunohistochemical stain showed partly positive for p53. Immunohistochemically, atypical cells were positive for CD56, synaptophysin, and INSM1 (Fig. 3C and D). The index of Ki-67, which was used to evaluate the grade of NET was 2.2%. Histological examination of the resected specimen revealed a mixed epithelial dysplasia, dominantly low grade and partly high grade, and NET, grade 1. The patient was finally diagnosed with gastric mixed adenoma and NET, grade 1.
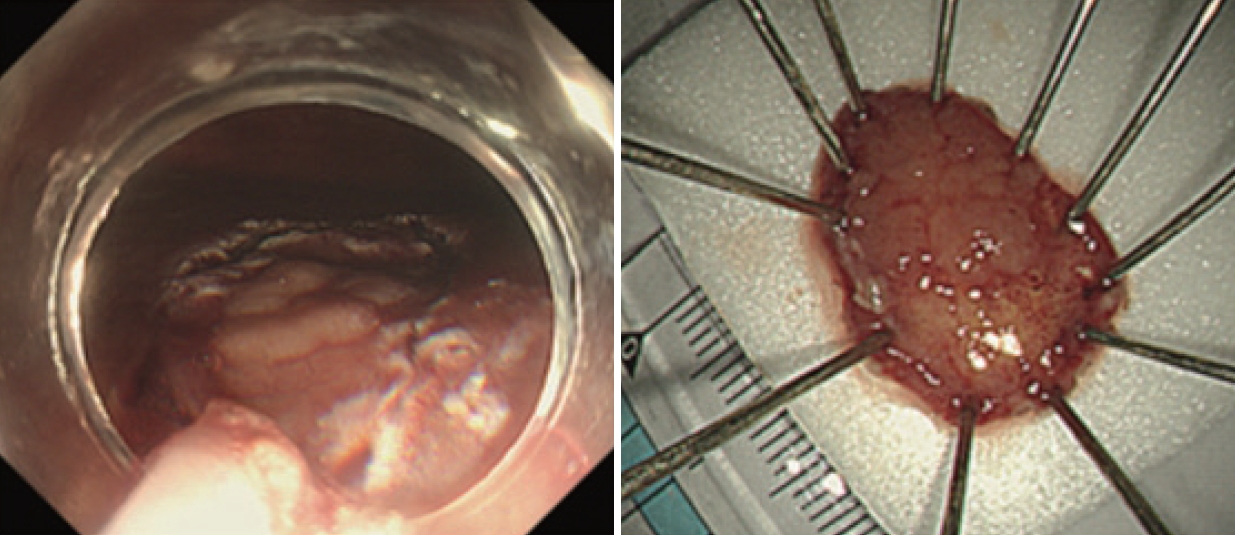
ESD was performed for the removal of gastric adenoma. The specimen size was about 20×20 mm. ESD, endoscopic submucosal dissection.
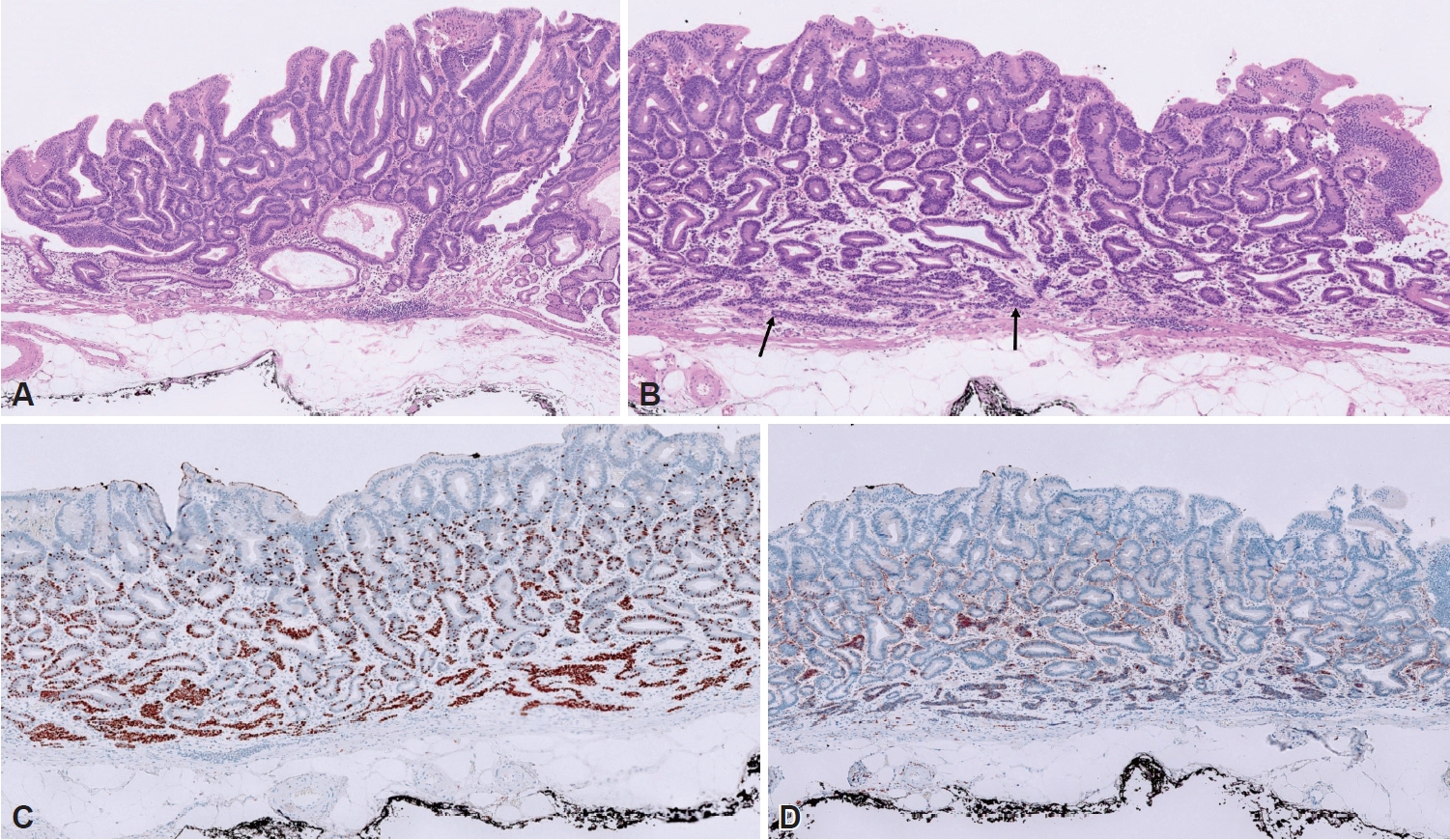
Microscopic finding of resected gastric MiNEN. A: H&E stain (×200) revealed epithelial dysplasia, dominantly low-grade. B: H&E stain (×200) revealed epithelial dysplasia with low grade with NET1 component (arrows). C: Immunohistochemical INSM1 stain revealed a positive result (stained brownish, ×200). D: Immunohistochemical CD56 stain revealed a positive result (stained brownish, ×200). MiNEN, mixed neuroendocrine- nonneuroendocrine neoplasm; H&E, hematoxylin and eosin; INSM1, insulinoma-associated protein 1.
There was no evidence of intra-abdominal or intra-thoracic metastasis in abdominopelvic computed tomography (CT) and chest examination. The patient has been followed up with upper gastrointestinal endoscopy and abdominopelvic CT on an outpatient basis until now for about 6 months without any evidence of recurrence.
DISCUSSION
In 1988, Moyana et al. [3] reported a complex glandular carcinoid tumor of the digestive tract. Since then, the definition and nomenclature of this lesion have varied. Many different terms (i.e., Composite carcinoid tumor, Multidirectionally differentiated carcinoma, Mixed adenocarcinoma tumor, etc.) had been used to define mixed epithelial neoplasms composed of NE and non-NE components. Thus, it leads to confusion among both clinicians and pathologists. In 2016, La Rosa et al. [4] proposed “mixed nonneuroendocrine and neuroendocrine neoplasm (MiNEN).” Introduced first for the pancreas by the 2017 WHO classification of tumors of endocrine organs, this term is used for all mixed neoplasms in the gastrointestinal system currently.
These types of tumors are very rare, accounting for only 1% of all malignancies that occur in the digestive tract [5]. MiNENs are a heterogeneous group of tumors whose prognosis and characteristics can vary depending on their detailed tumor composition. It is generally accepted that a tumor must contain two or more histologically distinct components, with one component exhibiting NET differentiation, and each component individually accounting for at least 30% of the total tumor volume to be classified as a MiNEN, but this cutoff value has been controversial since it was first proposed, as there have been no systematic studies to reaffirm the exact value of this prognostic definition [4,6,7]. Recent retrospective studies have shown that the prognosis of MiNEN depends on the degree of differentiation, not the volume ratio of the two components [8,9].
Mixed forms of gastric adenoma and NETs are rare, with only about a dozen case reports in our review, limiting our ability to analyze their characteristics and prognosis [7-17]. In the past, the term MANET has been proposed, and it is thought to have a relatively good prognosis by categorizing it as a low-grade MiNEN.
In the pathological aspect, its NE component is generally located within the deep central portion of the polyp, whereas the adenomatous component occupies most of the periphery.
In this case, a tubular adenoma with low-grade dysplasia was suspected based on endoscopic and histologic findings. However, after ESD in a relatively small lesion, a combination of lowgrade, high-grade adenomas and NETs were finally observed and diagnosed as MiNENs. Endoscopic differentiation of NE components within adenomas is very difficult, and an accurate diagnosis based on histologic specimens was thought to be difficult due to the presence of MiNENs-like features. At present, there are no therapeutic guidelines for gastric MiNENs. Treatment is determined by more invasive lesions among the two components, which have higher malignant potential. In this case, the non-NE lesion in the mucosa and NE lesions in the muscularis mucosa, with a total diameter of less than 20 mm. And regardless of the NET grade 1 component, there was a partial presence of a high-grade dysplastic component that did not invade the resection margin. Therefore, treatment and follow-up were performed according to high-grade dysplasia or typical gastric NET grade 1. In this case, we believe that endoscopic complete resection and regular follow-up would be appropriate. The prognosis of benign gastric MANET is not fully determined due to the rarity of cases at present. Complete endoscopic removal of the MiNENs would be considered curative because the contained NET component would be a main predictive factor to determine the prognosis.
This case shows that even if it is a lesion that endoscopically suspects pure adenoma or NET in clinical practice, there are the possibility of co-existing heterogeneous histopathologic components. Since there is no complete therapeutic consensus, future studies are needed to avoid poor prognosis.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author upon reasonable request.
Conflicts of Interest
Yeon Ji Kim who is on the editorial board of the The Korean Journal of Helicobacter and Upper Gastrointestinal Research was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflict of interest.
Funding Statement
None
Authors’ Contribution
Conceptualization: Yeon Ji Kim. Data curation: Kwon-Eui Hong. Formal analysis: Yeon Ji Kim. Investigation: Yeon Ji Kim. Methodology: Kwon-Eui Hong, Yoon Jung Choi. Supervision: Yeon Ji Kim, Yoon Jung Choi. Validation: Kwon-Eui Hong. Writing—original draft: Kwon-Eui Hong. Writing—review & editing: Yeon Ji Kim. Approval of final manuscript: all authors.
Ethical Statement
All procedures were conducted in compliance with the tenets of the Helsinki Declaration.
Acknowledgements
None