Is Ex Vivo Training before In Vivo Training Effective in Learning Gastric Endoscopic Submucosal Dissection?
Article information
Abstract
Background/Aims
The learning curve is essential in endoscopic submucosal dissection (ESD) training to improve outcomes and reduce the risk of procedure-related complications. We compared the outcomes of gastric ESD in live pigs performed by inexperienced endoscopists with or without ex vivo training.
Materials and Methods
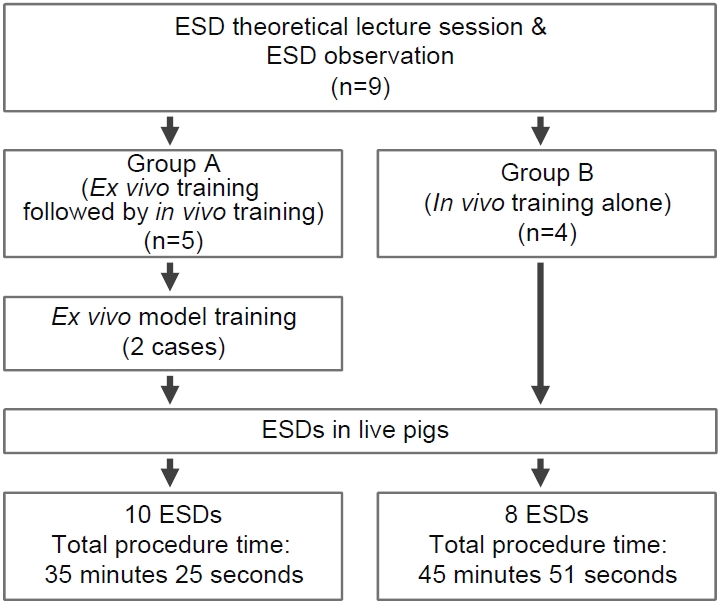
At the Olympus Medical Training and Education Center, nine endoscopists inexperienced in ESD were randomly divided into two groups (group A: ex vivo training followed by in vivo training; group B: in vivo training only), and they performed gastric ESDs.
Results
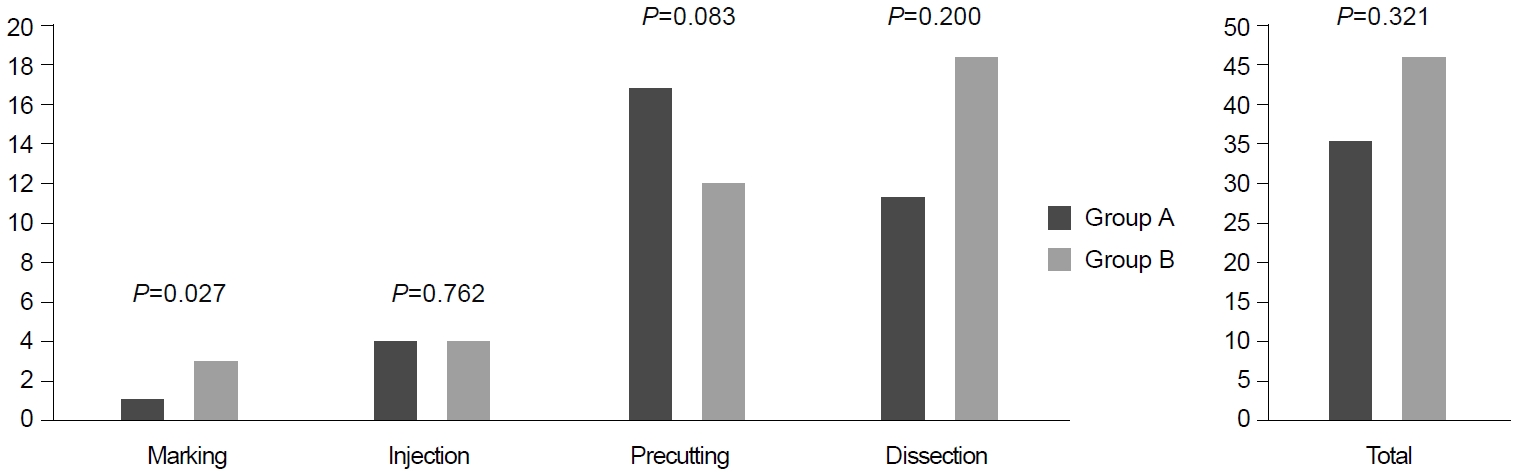
A total of 18 ESDs were performed. The en bloc resection rate was 88.9% (16/18), and the complete resection rate was 94.4% (17/18). The median specimen size was 2.5 cm in group A and 2.1 cm in group B (P=0.227). There was no significant difference in the procedure time between the two groups, except for the marking time (0′58″ vs. 2′58″, P=0.027). However, group A took a shorter time in dissecting the same area than group B (109 vs. 246 sec/cm2, P=0.083). Complication rates were not significantly different between both groups.
Conclusions
The procedure time during in vivo ESD training in pigs may be shortened by prior ex vivo training. However, the ex vivo model presented poor air inflation, unstable fixation, and excessive mucosal hardness for cutting. An advanced simulator or sufficient ex vivo training may be effective in training for the ESD procedure.
INTRODUCTION
Endoscopic submucosal dissection (ESD) is a standard method for the treatment of early gastric cancer, and its efficacy and safety in expert’s hands have been confirmed [1,2]. ESD rather than endoscopic mucosal resection is preferred to achieve higher en bloc and curative resection rates in addition to lower local recurrence rates [3,4]. However, because ESD is a highly operator-dependent technique, there have been attempts to determine the optimal training system. Some researchers have recommended practicing on approximately 30 cases as a requirement for a quality-controlled procedure [5,6], and other experts from Europe have suggested requiring a competent level of hands-on experience in live pigs before beginning its application in humans to overcome the issues regarding the learning curve [7]. In addition, a strategy for learning ESD, followed by training in harvested porcine stomachs and subsequently in live pigs, has been reported [8].
Currently, a standard training system remains unestablished, although some trials have been conducted to facilitate the learning curve by training using ex vivo and/or in vivo animal models [9,10]. Therefore, this prospective study aimed to compare the outcomes of gastric ESD in live porcine between two groups, with and without the ex vivo porcine training.
MATERIALS AND METHODS
1. Baseline characteristics of participants
Nine endoscopists participated in this study in November 2019, who were clinical fellows in their first (n=7) and second years (n=2) at the time. All participants received ESD theoretical session 1 week before the training and observed at least two ESD procedures. None had experience in performing ESD on patients. All participants were affiliated with the Department of Gastroenterology.
The nine participants were classified into two groups based on their previous experience in esophagogastroduodenoscopy (EGD). There was no significant difference in the number of performed diagnostic EGD between the two groups (P=0.556). Five participants were included in group A, which underwent ex vivo training followed by in vivo training wherein ESD was performed in a live porcine model after two sessions of ex vivo training using harvested porcine stomachs. The other four participants were included in group B, who underwent only in vivo training. Fig. 1 shows the flow of the study. This study was approved by the Institutional Animal Care Use Committee (number: KTEC-2019-002).
2. Preparation of pigs for ESD
The study was conducted at the Olympus Medical Training and Education Center in a fully equipped endoscopic unit. Both groups of endoscopists participated in a 1-day (4 h/day) training session for gastric ESD. Experienced tutors supervised the participants.
1) Ex vivo model
Five harvested porcine stomachs with esophagus were prepared in a plastic box with a hole in one of the short sides. Stomachs with the entire esophagus still attached were obtained. Each stomach was placed above a metal plate in the plastic box. An overtube was introduced into the hole and inserted into the esophagus. Plastic clamps were used to tighten the esophagus to the overtube and prevent it from sliding with the movements of the endoscope. A dedicated endoscope (GIF-290HQ; Olympus, Tokyo, Japan) was used for all procedures in this study. Each of the participants in group A performed two ESDs.
2) In vivo model
Four live mixed-breed female pigs weighing 30~35 kg were used. The pigs were fasted for 24 hours before the ESD procedure. General anesthesia was administered during the entire procedure. An overtube was used to prevent trauma of the larynx during multiple sessions of ESD. Intramuscular ketamine/tiletamine/zolazepam was administered as a premedication. Induction was accomplished by inhalation anesthesia with sevoflurane. The pigs were monitored by the veterinary staff during the entire procedure.
3. Creating target lesions in ex vivo and in vivo training models
Target lesions in both harvested stomachs and live pigs were created by placing marking dots on the gastric mucosa using the tip of a dual knife (KD-650L; Olympus) measuring approximately 10~15 mm in size by three experienced endoscopists. The participants were asked to mark the periphery with approximately 5-mm safe margins outside the target lesion.
4. Endoscopic procedures
The ESD procedures were similar to the standard protocol conducted in humans. Fig. 2 shows the ESD procedure in the ex vivo and in vivo models. ESD was conducted in the anterior, posterior, and greater curvature sides of the body or the antrum of the stomach. Olympus GIF-HQ290 gastroscope was used during the procedure, and a transparent cap was applied to the tip of the endoscope. A dual knife (KD-650L; Olympus) was used for marking. After marking, a submucosal injection with normal saline mixed with hyaluronic acid and indigo carmine was administered to lift the lesion. The starting point of precutting was made using a needle knife (Olympus). An insulated-tip knife (KD-611L; Olympus) was used for circumferential precutting and dissection of the submucosal layer. All resected specimens were pinned on a plastic plate and then measured.
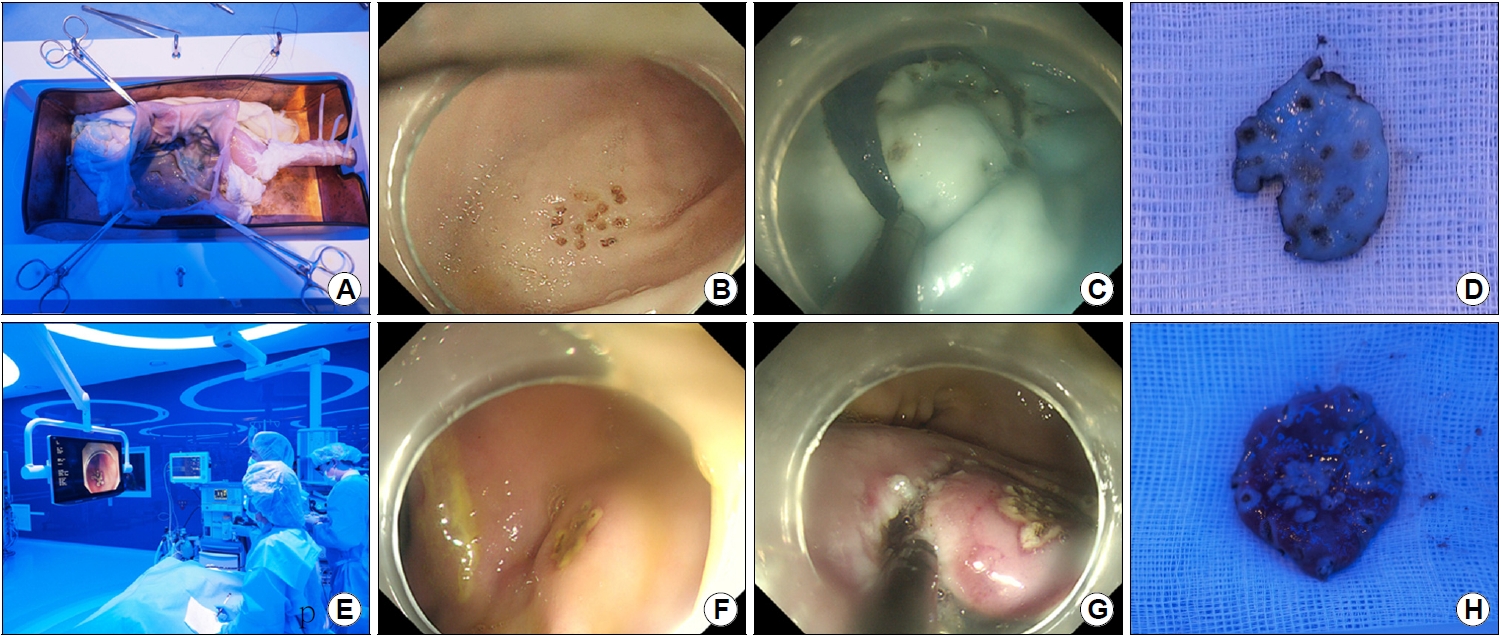
Endoscopic submucosal dissection (ESD) training in ex vivo (A-D) and in vivo model (E-H). (A) An open ex vivo harvested porcine stomach after ESD training. (B) Target lesion is artificially created using the tip of a dual knife in ex vivo porcine stomach. (C) Precutting is performed in ex vivo porcine stomach. (D) Dissected specimen of group A. (E) ESD in live pig is performed by a trainee. (F) Target lesion of live porcine stomach. (G) Submucosal dissection is performed on live porcine stomach. (H) Dissected specimen of live pig.
5. Outcome measurements
The nine trainees performed 18 resections on four pigs. After completing two gastric ESD in the ex vivo models in group A, all trainees performed two gastric ESD in the in vivo models. The following variables were prospectively recorded: 1) location of the target lesion; 2) time required for marking, injection, precutting, dissection, and hemostasis; 3) size of the resected specimen; 4) completeness of the resection (complete en bloc, complete piecemeal, and incomplete); and 5) complications (bleeding and perforation). The primary endpoint of this study was the procedure time between the two groups, with or without the ex vivo porcine training model, measured from the beginning of precutting until dissecting lesion from gastric wall. Secondary endpoints were post-procedural bleeding, perforation, and en bloc resection rate.
6. Questionnaires on ex vivo and in vivo training for ESD
At the end of the training, all participants evaluated their own performance and difficulty score for the ESD procedure using 5-score scales (from 1=very ineffective to 5=very effective). The questionnaire consisted of the effectiveness of theoretical sessions, effectiveness of ESD observation, effectiveness of the ex vivo model, appropriateness of the number of ESDs in the ex vivo model, difference between ex vivo and in vivo training models, complicated steps of the ESD procedure, and difficult location of the ESD.
7. Statistical analysis
Continuous variables were presented as mean and standard deviation, and the Student’s t-test was used to analyze the variables. A chi-square or Fisher’s exact test was used to compare the categorical variables. Continuous variables were compared using the nonparametric Mann-Whitney U test. All statistical analyses were performed using the SPSS Statistics version 21.0 (IBM Corp., Armonk, NY, USA), and values of P<0.05 were considered statistically significant.
RESULTS
1. ESD outcomes
A total of 18 live porcine ESD procedures were performed by the nine endoscopists, with two cases per participant. Table 1 shows the results of the ESD procedures. The median procedure time of injection, precutting, dissection, and total procedural time showed no significant differences between group A and group B (Fig. 3). However, the time for marking was significantly shorter in group A than in group B (0′58″ vs. 2′58″, P=0.027). Regarding the ESD location, 60% of ESDs in group A and 50% of ESDs in group B were performed in the gastric body, with no significant locational differences.
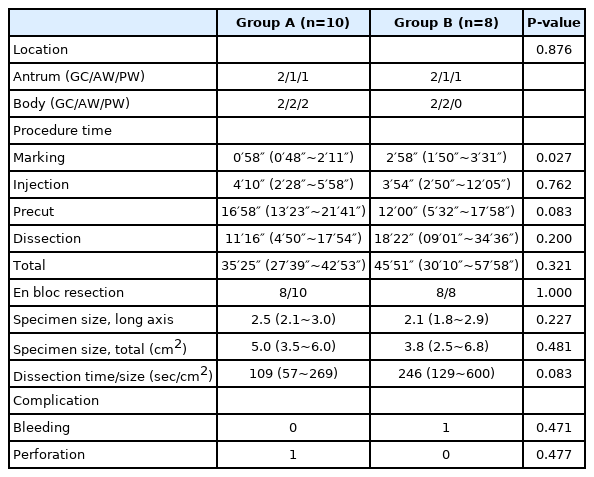
Comparison of the Data for Group A (Ex Vivo Training Followed by In Vivo Training) and Group B (In Vivo Training Only)
The resection was completed in 17/18 (94.4%) cases, except in one case in group A because of perforation. En bloc resection was achieved in 16/18 (88.9%) cases, except in one case of perforation and one case of piecemeal resection. The median size of the resected specimens was 5.0 cm2 (3.5~6.0) in group A and 3.8 cm2 (2.5~6.8) in group B, and there was no statistical difference between the two groups. In addition, the ex vivo training group took a shorter time to dissect the same area. One case required hemostasis after ESD due to bleeding, and it was easily managed without hemodynamic instability. Perforation was observed in were considered stat case in group A, and it was closed by clipping during the procedure. The time for closing the perforated site was not included in the procedure time analysis.
2. Participant opinions about ex vivo and in vivo training models
Tables 2-4 and Fig. 4 present the opinions of the participants on the efficacy of using ex vivo and in vivo porcine models in ESD training. Although they agreed with the feasibility of ESD training using the ex vivo harvested porcine stomach model, significant differences were noted in performing ESD between the ex vivo and in vivo models in terms of air inflation, mucosal hardness, mucosal lifting, and fixation. The most challenging step of ESD was precutting (n=6) and dissection (n=3), and the most difficult location for ESD was typically the anterior and posterior walls of the stomach in both ex vivo and in vivo models.

Mean Score of the Answers to the Questions of the Ex Vivo and In Vivo Training for ESD: Effectiveness of Training
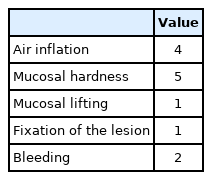
Mean Score of the Answers to the Questions of the Ex Vivo and In Vivo Training for ESD: Difference between the Ex Vivo and In Vivo Training (Multiple Answers Possible)

Number of the Answers to the Questions of the Ex Vivo and In Vivo Training for ESD: Most Difficult Location for ESD
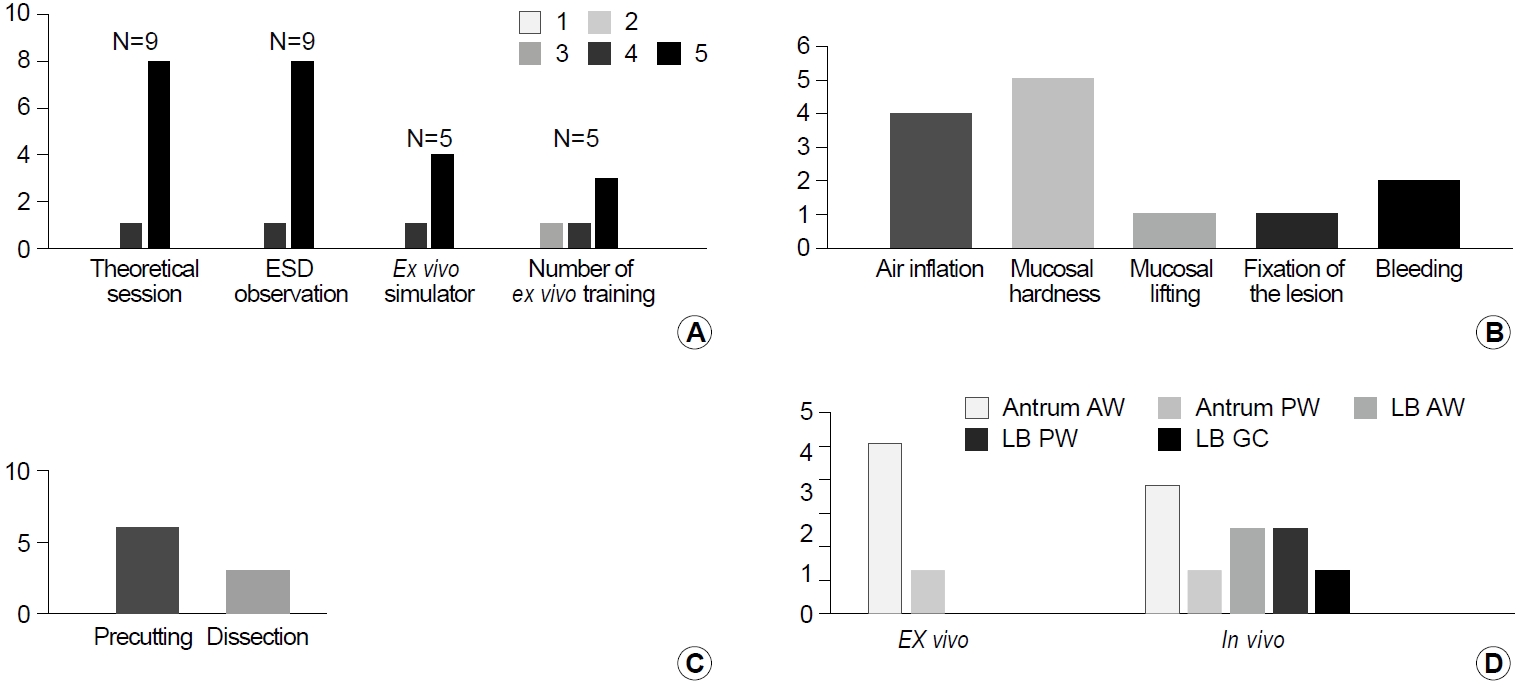
Questionnaires on the ex vivo and the in vivo training for endoscopic submucosal dissection (ESD). (A) Efficacy of training session. Scale, 1 (not effective) to 5 (very effective). (B) Difference of technical experience between the ex vivo and in vivo training. (C) The most difficult step during ESD. (D) The most difficult location for ESD. AW, anterior wall; PW, posterior wall; LB, low body; GC, greater curvature.
DISCUSSION
ESD has become a treatment of choice for early gastric cancer according to the consensus criteria, and there have been efforts to learn the technique in a short term with a systemic curriculum. However, a standardized program for ESD training has not yet been established. Several researchers recommend practice on live animal models, in which the procedural steps of ESD and the management of complications, including bleeding and perforation, can be imitated before practicing on humans [11-14]. However, live animal models have some limitations due to requirements for veterinarians, expensive instruments, special facilities, and consideration of ethical principles. The ex vivo model is advantageous in terms of cost and convenience for training. In this study, we investigated the efficacy of the conventional ex vivo model for accelerating the educational impact of gastric ESD training in a live animal model. We found no significant differences were noted between the group with ex vivo training followed by in vivo training and the group with only in vivo training, except for the shortening of the procedural time of marking.
ESD was developed in Japan, and a basic model of ESD training in Eastern countries is the classic mentor-apprentice teaching model. On the other hand, in Western countries, the lack of cases and local experts is the major limitation for learning ESD [13-15]. Berr et al. [16] reported that the en bloc resection rate and the curative resection rate of untutored ESD in the West were 76% and 63%, respectively. In addition, Zhang et al. [17] reported that the learning curve of untutored ESD in the United States was 170, 150, and 280 cases for lesions of the esophagus, stomach, and colon, respectively. Therefore, reports on the feasibility of in vivo and ex vivo porcine models have been proposed.
Our results showed that an ex vivo model for gastric ESD training did not significantly improve the educational impact of training using an in vivo model. Several problems were found in the ex vivo model for ESD training. First, the ex vivo model was kept frozen and then melted on the training day during the preparation process. Similarly, Parra-Blanco et al. [8] and Wang et al. [18] reported that the ex vivo porcine stomach appeared to be harder than the human stomach. Because of the tissue hardness of the ex vivo porcine stomach, the participants needed more powerful maneuvers and electric energy for precutting or dissection. This may cause perforation, which is a severe adverse event of the ESD procedure. In this study, perforation in the in vivo model was made only in group A. Moreover, these stomachs required a repeat submucosal injection. Second, the stomach part of the ex vivo model was unfixed and frequently moving. After air inflation to the ex vivo model for the ESD procedure, it was rotated or more movable than the expected range. The participants required additional movements during endoscopy, including the use of two hands, for targeting the lesion during the ESD procedure in the ex vivo model. Finally, the ex vivo model was difficult to maintain air inflation despite tightly clipping the end of the ex vivo model.
On the other hand, these problems can be experienced in human ESD, such as poor air inflation due to poor patient cooperation and difficulty targeting due to breath. In addition, experts have recommended five or less cases of gastric ESDs in an ex vivo model for trainees before practicing on human cases [15]. We performed two sessions of ESD training using the ex vivo model in group A, and no significant improvement in procedure time was observed in group B. It is unclear whether more than two ESDs in the ex vivo model would better demonstrate the effect of ex vivo training. Furthermore, despite the lack of statistical significance, the submucosal dissection time of the same area tended to be shorter in group A than in group B, which might be considered that training in the box simulator was helpful. On the other hand, the precutting time was rather longer in group A, which is presumed to be affected by the location of the lesion.
Recently, some authors have demonstrated the efficacy of using live animal models for gastric ESD training [11,19,20]. Although the efficacy of using ex vivo models for ESD training in the esophagus or colorectum has been reported, there are no reports on the efficacy or benefits of using the ex vivo model for live animal models or human gastric ESD training [21,22]. Because of the limitations of the live animal model, including the expensive cost or ethical considerations, we investigated the efficacy of the ex vivo model in ESD training.
Trainees in this study reported a high score of efficacy of the ex vivo training in the questionnaire. The inexperienced trainees used the instruments and accessories during the ESD procedure for the first time, especially the endoscopic knife. For these participants, the ex vivo training was a good opportunity for conducting ESD without the risk of bleeding and perforation. Several guidelines recommend ESD training on ex vivo or live animal models before practicing on human cases [13-15,23]. This is useful to gain the basic ESD skills and competence in the ESD procedure.
This study had some limitations. First, the target sites in live porcine were not matched between the two groups, despite the lack of statistically significant differences. Due to the difficulty to procure a sufficient number of live porcine for the study, the participants conducted ESDs on the anterior wall, the posterior wall, and the greater curvature of the stomach. Second, the number of ex vivo ESD was not sufficient and the study sample was small. Live animal models require expensive instruments and special facilities and have ethical issues. Therefore, we investigated the efficacy of the ex vivo model, which is inexpensive and relatively convenient for preparing. Although two sessions of ex vivo training was insufficient, it enabled participants to achieve competence in using instruments. The number of sufficient ex vivo training for the porcine ESD model has not been established yet; thus, further study is needed to evaluate its effect.
In conclusion, the role of ex vivo training in improving the educational effect for gastric ESD training in the in vivo porcine model was limited in this study. Although the number of ex vivo training may have been sufficient to learn using instruments, it may have been insufficient to improve the learning curve. Considering that the total procedure time, especially marking and dissection time, was shorter in the ex vivo training group, repetitive ex vivo training may improve ESD skills. Further studies are required to develop an effective ESD training system using ex vivo and in vivo models.
Notes
No potential conflict of interest relevant to this article was reported.