Risk of Peptic Ulcer Bleeding Associated with Helicobacter pylori Infection, Nonsteroidal Anti-inflammatory Drugs, and Low-dose Aspirin Therapy in Peptic Ulcer Disease: A Case-control Study
Article information
Abstract
Background/Aims
The association between Helicobacter pylori infection and nonsteroidal anti-inflammatory drugs (NSAIDs) or low-dose aspirin therapy as a risk factor for peptic ulcer bleeding (PUB) remains unclear. This study investigated the risk of PUB associated with H. pylori infection and NSAID or low-dose aspirin therapy in patients with PUD.
Materials and Methods
This case-control study investigated 340 patients with PUB between 2012 and 2016. The control group comprised age and sex-matched patients with endoscopically documented non-bleeding ulcers. Using logistic regression analysis, the adjusted odds ratio (AOR) was calculated for the risk of PUB.
Results
Of the patients investigated, 57.9% in the study group and 51.8% in the control group were diagnosed with H. pylori infection (P=0.106). Logistic regression analysis showed synergistic interaction between H. pylori infection and low-dose aspirin therapy. Multivariate analysis showed that low-dose aspirin (AOR 3.92, P=0.001), NSAIDs (AOR 2.98, P=0.001), warfarin (AOR 14.57, P=0.011), gastric ulcer (compared with duodenal ulcer) (AOR 1.65, P=0.01), and smoking (AOR 1.97, P=0.004) increased the risk of PUB compared with the risk of PUD.
Conclusions
Both NSAIDs and aspirin are independent risk factors for bleeding in patients with PUD. Additionally, low-dose aspirin therapy concomitant with H. pylori infection produced a synergistic effect. Therefore, H. pylori eradication may be crucial in aspirin users. Moreover, a proton pump inhibitor should be prescribed in patients with a history of bleeding ulcers who need long-term NSAID treatment.
INTRODUCTION
Helicobacter pylori infection and the use of non-steroidal anti-inflammatory drugs (NSAIDs) including aspirin (acetylsalicylic acid, ASA) represent well-known risk factors for peptic ulcer disease (PUD) [1]. Over the recent decades, as the rate of H. pylori infection decreases, the incidence of PUD also decreases worldwide [2]; however, only a slow decrease was seen in the rate of hospitalization caused by peptic ulcer bleeding (PUB) [3]. Moreover, an increasing old age population with cardiovascular disease or arthritis showed an increasing evidence of H. pylori-negative and NSAIDs-negative idiopathic ulcer disease [4].
In a systematic review, the pooled relative risk (RR) for NSAIDs-related gastrointestinal (GI) bleeding was 4.50 (95% confidence interval [CI]: 3.82∼5.31) and the RR of aspirin-related GI bleeding was 2.07 (95% CI: 1.61∼2.66) [5]. Most clinical guidelines mentioned that H. pylori infection and NSAIDs are independent risk factors for the development of PUD and guidelines recommend testing for H. pylori in users of aspirin and NSAIDs with a history of peptic ulcer [1,6-8].
In daily clinical practice, the concomitant use of NSAIDs or aspirin in H. pylori-infected subjects is common, especially in elderly patients. Several case-control studies have tried to understand the relationship between H. pylori infection, and NSAIDs or aspirin; however, interaction between H. pylori infection and NSAID/aspirin and role of H. pylori eradication in drug users remains inconclusive [9-11]. A recent epidemiological study has shown that H. pylori infection and concomitant use of NSAIDs have a synergistic effect on the risk of PUB [12]. However, the interaction between H. pylori and low-dose aspirin is poorly defined and the results are more controversial when compared with NSAIDs [13]. Further, most previous studies compared between PUB and normal control, therefore, it is needed to be clarified about bleeding risk in patients with PUD.
The risk of bleeding in PUD subjects with H. pylori infection taking concomitant NSAIDs or low-dose aspirin remains unclear and several studies addressing this issue drew inconclusive results. Hence, this study aimed to determine the interaction between H. pylori and NSAID/ASA and to identify independent factors related with bleeding in patients of PUD.
MATERIALS AND METHODS
1. Study design and patients
This was a hospital-based case-control study performed at the Kangdong Sacred Heart Hospital (IRB no. 2017-12-011-001). We recruited consecutive patients with PUB admitted to our institution from 2012 to 2016. The study group was PUB patients who complained of melena or hematemesis at admission and underwent endoscopy within 24 hours of admission. The control group was patients with an endoscopic diagnosis of PUD without bleeding and was matched for age and sex with the PUB group. PUD was defined as a mucosal break, at least 5 mm in diameter, with visible depth assessed by an endoscopist. In most patients, biopsy specimens were taken from the edge of the ulcer to exclude malignancy in the gastric ulcer.
In the PUB group, exclusion criteria were as follows: (1) patients who had bleeding from areas other than the peptic ulcer such as gastric or esophageal varices, upper GI malignancy, angiodysplasia, Mallory–Weiss syndrome; (2) patients who had taken antibiotics or proton pump inhibitor (PPI) within the last one month of enrollment; (3) patients with coagulopathy; (4) patients with liver cirrhosis; and (5) patients who had a history of PUB.
The PUD group comprised age (±5 years) and sex-matched, non-bleeding ulcer patients who visited the outpatient unit during the same period as that of the PUB patients. In the PUD group, subjects who had taken antibiotics or PPI within the last one month of enrollment. To exclude patients with ulcer bleeding, patients with active-stage ulcer on endoscopy were excluded in PUD group. We reviewed medical records and collected clinical information such as drug history, smoking, alcohol history, and underlying disease. Current NSAIDs or aspirin use was defined as at least one dose taken within 4 weeks before the index date of endoscopic procedure. Low-dose aspirin was defined as a dose no greater than 300 mg/day. In antiplatelet agents, clopidogrel was included in 95% of total patients and only warfarin other than direct oral anticoagulant was included. We defined the patients who were presently smoking as ‘smokers’ and the patients who consumed more than 40 g of alcohol a day in men and over than 20 g a day in women as ‘alcoholics.’
2. H. pylori test
H. pylori infection was assessed by rapid urease test (CLOtest, Pronto Dry New; Medical Instruments Corp, Herford, Germany) in all subjects. A typical change in color on rapid urease test was defined as H. pylori infection. In patients of PUB with negative rapid urease test, a serologic test was performed, or the rapid urease test was repeated at the time of follow-up endoscopy to confirm H. pylori infection.
3. Statistical analysis
All data were analyzed using SPSS software for Windows, version 19.0 (IBM Corp., Armonk, NY, USA). Univariate and multivariate analysis were performed to compare clinical features between the PUB and PUD groups using the chi-square test or Fisher’s exact test for categorical variables and independent sample t-test for continuous variables. Conditional logistic-adjusted regression analyses were carried out to compute RRs and 95% CI, similar to that in a recent study [12]. Multivariate analysis was performed in statistically significant factors of univariate analysis. A two-sided P value less than 0.05 was considered statistically significant.
RESULTS
In all, 680 patients were enrolled in this study. The median age of patients was 58 (range: 19∼88) years and 74.4% of patients were male. H. pylori infection was noted in 54.9% of all subjects.
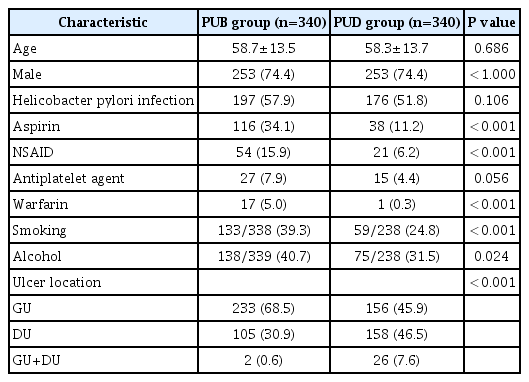
1. Comparison of the clinical characteristics between PUB group and non-bleeding PUD group
Table 1 shows the comparison of baseline characteristics between the PUB and PUD patients. The proportion of H. pylori infection was not statistically different between the two groups (PUB vs. PUD, 57.9% vs. 51.8%; P=0.106). In the PUB group, there were more patients taking aspirin, NSAIDs, and anticoagulants. Moreover, there were more smokers and alcoholics in the PUB group. The location of ulcer was different between the PUB and PUD groups. As shown in Table 1, gastric ulcers (GU) were found in 68.5% of PUB patients and 45.9% of PUD patients (P=0.001).
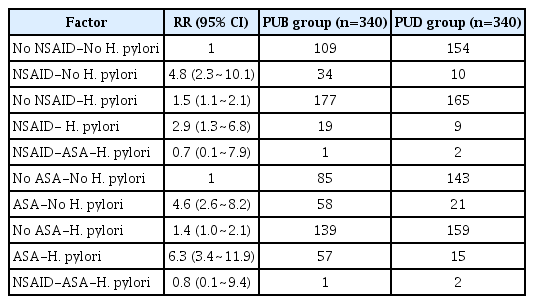
2. Interaction of H. pylori infection with NSAIDs or aspirin
Table 2 describes the RR for bleeding with respect to NSAIDs or low-dose aspirin and H. pylori status in PUD patients. If the RR for bleeding in patients with no intake of NSAIDs or aspirin and with no H. pylori infection is considered as a reference value of 1, the RR for bleeding in patients with H. pylori infection and taking NSAIDs, was less than a simple additive effect of NSAIDs and H. pylori infection. However, there was a synergistic effect of low-dose aspirin and H. pylori infection.
3. Multivariate analysis of the risk factors of bleeding, compared with non-bleeding PUD
To evaluate independent risk factors for bleeding in subjects with PUD, we conducted a logistical regression analysis. On multivariate analysis, low-dose aspirin (adjusted odds ratio [AOR] 3.92, P=0.001), NSAIDs (AOR 2.98, P=0.001), warfarin (AOR 14.57, P=0.011), gastric ulcer rather than duodenal ulcer (AOR 1.65, P=0.01) and smoking (AOR 1.97, P=0.004) increased the risk of PUB compared to the risk of PUD (Table 3).
DISCUSSION
In the present case-control study, we investigated the interaction between H. pylori infection and NSAIDs or aspirin use and the risk factor for bleeding in patients with PUD. Both NSAIDs and aspirin were independent risk factors for bleeding in patients with PUD and there was a synergistic effect of low-dose aspirin and H. pylori infection. On multivariate analysis, low-dose aspirin (AOR 3.92, P=0.001), NSAIDs (AOR 2.98, P=0.001), warfarin (AOR 14.57, P=0.011), gastric ulcer rather than duodenal ulcer (AOR 1.65, P=0.01) and smoking (AOR 1.97, P=0.004) increased the risk of PUB compared to the risk of PUD.
Until now, there have been several studies exploring the synergistic effect of NSAIDs or aspirin with H. pylori infection; however, the results have been controversial [5,10,12-16]. The major reason could have been the different study designs and heterogeneous patient populations. In 2015, Sostres et al. [12] conducted a large case-control study including 666 cases of PUB and 666 as controls. They concluded that there was a synergistic effect between only NSAIDs and H. pylori infection. This study compared patients with PUB and controls without a peptic ulcer. Similarly, most of the case-control studies compared patients of PUB with non-ulcer patients as the control group [14,16].
In contrast, Okan et al. [15] compared 96 patients with bleeding ulcers and 106 patients with non-bleeding ulcers and the result showed no synergistic effect between H. pylori and use of NSAIDs. The authors contended that a bleeding peptic ulcer is just a complication of peptic ulcer; hence, the comparison of patients with bleeding ulcer with non-ulcer patients is not appropriate to study the risk for bleeding in PUD [15]. To that point, our study was relatively large-scaled study to investigate the interaction between aspirin or NSAIDs and H. pylori infection in PUB compared with PUD, not normal control.
Our study showed no synergistic interaction between NSAIDs and H. pylori. The interaction of mechanisms between H. pylori and NSAIDs is not well understood. It has been suggested that H. pylori infection could protect against, and even accelerate the healing of NSAIDs-induced ulcers because of acid suppression caused by H. pylori induced pangastritis, especially in the presence of PPI [5,17]. Additionally, H. pylori infection results in prostaglandin production by the gastric mucosa, which might be protective against superficial mucosal injury [18], although it has not been conclusively proven. According to the meta-analysis in 2005, H. pylori eradication appeared to be effective only in NSAIDs-naïve patients, while in chronic NSAIDs-users, maintenance with PPI might be more effective than H. pylori eradication alone [9]. Our study included patients who had taken NSAIDs within 4 weeks before enrollment, however, we could not specify the duration or dose of NSAIDs, which could have influenced the results.
There are few literatures about the interaction between aspirin and H. pylori infection. A recent systematic review including 13 studies reported that no definite conclusion could be drawn regarding the impact of H. pylori on upper GI bleeding risk in aspirin users, because most of the included cohorts were heterogeneous [19]. Aspirin is non-selective inhibitor of cyclooxygenase (COX), which suppresses prostaglandin synthesis and thromboxane A2. This irreversible nature of COX inhibition and its antithrombotic effect differentiates low-dose aspirin from NSAIDs. These differences might explain why low dose aspirin has a lower risk of gastric ulcer compared to NSAIDs; however, it increases the risk of bleeding from pre-existing ulcers such as those caused by H. pylori [5,13]. Hence, H. pylori might have a more significant role in aspirin-induced PUB than in NSAIDs-induced PUB [5]. In our results, there was a synergistic effect of low-dose aspirin and H. pylori infection, therefore H. pylori eradication may be crucial to prevent aspirin-induced PUB.
Most guidelines recommend that H. pylori eradication alone might not be sufficient as a risk reduction strategy in patients with a history of an ulcer-related complication, who require subsequent therapy with NSAIDs or aspirin. Concomitant therapy with PPI in patients with a high risk for recurrence of an ulcer-related complication has been recommended [1,6,8]. Our study suggests that prevention strategies with PPI in PUD might be necessary in chronic NSAIDs-users.
On multivariate analysis, NSAIDs and aspirin were independent risk factors for bleeding, in patients with PUD. The result was concordant with results from previous studies [20,21]. However, H. pylori infection was not a significant factor for PUB in our study. The association between H. pylori infection and PUB was previously studied in a meta-analysis, which confirmed that H. pylori infection increased the risk of ulcer bleeding (odds ratio: 1.79) [11]. In our study, the frequency of H. pylori infection in PUB patients was lower than that in previous studies (57.9% vs. 72%) [22]. It can be explained by the difference in diagnostic methods for H. pylori and the distribution of the ulcer location. In general, the sensitivity of rapid urease test in bleeding patients is known to be lower than that in non-bleeding patients (85% vs. 92%), while histology is the most reliable test in cases of PUB [23]. However, in our study, limited by its retrospective design, we performed rapid urease test in all patients and a serologic test or repeated rapid urease test was performed in PUB groups.
Additionally, in our PUB population, the proportion of GU was higher than duodenal ulcers (DU) (68.5% vs. 30.9%) and the proportion of DU was quite lower than that in previous studies (30.9% vs. 40~59%) [12,15,20]. A recent meta-regression study showed that the variability in the prevalence of H. pylori infection in PUB could be attributed to different diagnostic methodologies and to the patients’ characteristics and the proportion of DU [22].
This study has some limitations. First, it was a retrospective study; therefore, it might have a potential bias. To minimize the bias, the PUD group was selected from patients who were diagnosed with PUD during the same period as those in the PUB group and consecutively enrolled. Second, there might be a recall bias about the drug exposure history especially in the PUD group since they visited the outpatient units. This could have resulted in an underestimated proportion of drug intake in the PUD group and we could not identify exact drug dose or duration. Third, as mentioned above, we could not perform secondary method for H. pylori test in PUD group. Despite limitations, our study was relatively large-scale case-control study to investigate the interaction between aspirin or NSAIDs and H. pylori infection in PUB compared with PUD. Considering that the intake of aspirin and NSAIDs is increasing in old people, our study indicates changing trends in the characteristics of PUD and PUB.
In conclusion, both NSAIDs and aspirin are independent risk factors for bleeding in patients with PUD and synergistic interaction was observed between H. pylori infection and low-dose aspirin. Therefore, H. pylori eradication may be crucial for aspirin-users, and patients with a history of bleeding ulcers who need long-term treatment with NSAIDs may be needed to be prescribed a PPI [24].
Notes
No potential conflict of interest relevant to this article was reported.